Friday July 11th, 2025, in Kennedy Park, Lewiston Maine. More details for the 2025 event to come!
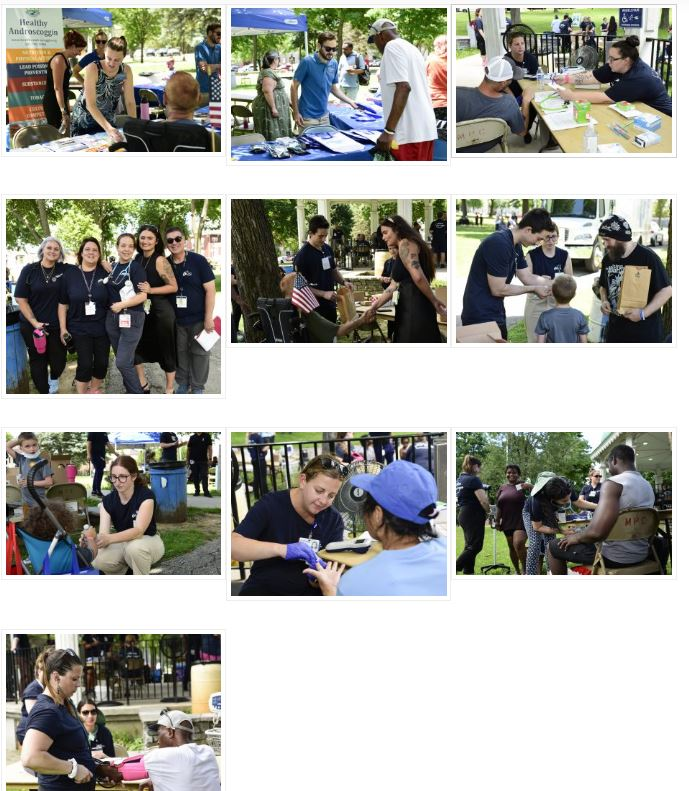
Photos from 2024’s Clinic in the Community
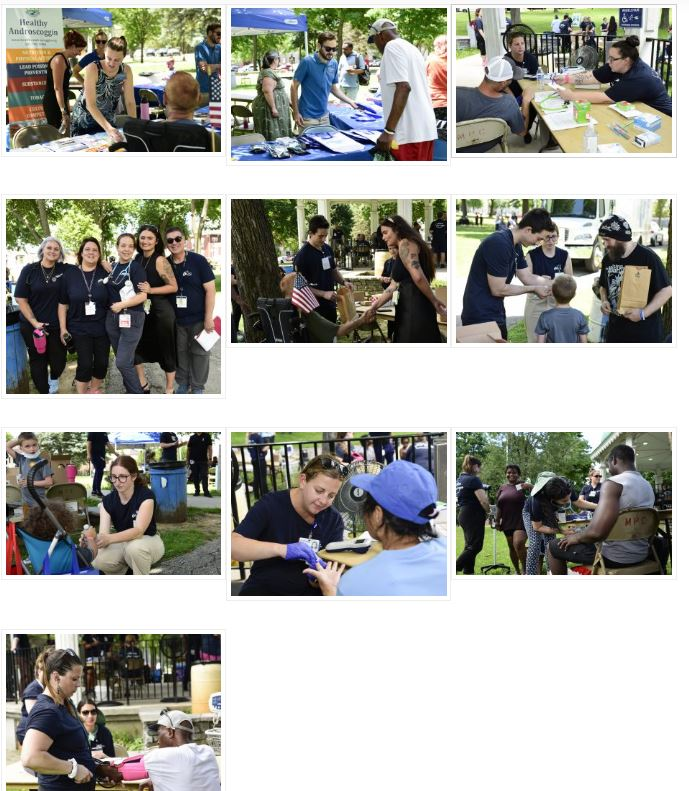
Photos from 2024’s Clinic in the Community
Mission: To train residents to competently triage, diagnose and treat a wide variety of medical concerns commonly seen in low resource settings which includes but is not limited to wilderness and international areas, while empowering residents with the tools to push their boundaries of knowledge when it comes to providing care in such settings.
Goal 1: Develop the ability to provide medical care performed in low resource and stressful situations with appropriate attention to detail (PROF 2).
Objectives:
Goal 2: Demonstrate an ability to optimize resources available in low resource situations (MK1, PC5).
Objectives:
Goal 3: Formulate a learning plan independently related to an area of low resource medicine that has special interest to you (PBL2).
Objectives:
Goal 4: Integrate knowledge obtained through clinical and didactic settings to maximize the chance of survival of self and party/patients under your care in a wilderness setting (MK1, PC5).
Objectives:
Goal 5: Perform basic improvised medical procedures and protocols with reasonable confidence and motor skills when in low resourced settings (PC5).
Objectives:
Goal 6: Be prepared to give recommendations for patients who will be in situations where they will not have access to the resources of CMMC or similar hospital (PC3).
Objectives:
Goal 7: Develop illness scripts for common causes of morbidity and mortality in low resource settings (PC1).
Objectives:
Using WIMP Funds: After using WIMP funds, the resident will be required to do a presentation on their trip/learning. If WIMP funds are used for an Away-away rotation, that doesn’t mean CME funding for that rotation is approved as well. That would also require approval from the PD. If you get approval to also use CME funding, the expectation is within 3 months of returning, you do a presentation that includes a review of the literature and evidence for an intervention or problem addressed, you saw on the trip. Those presentations should be reviewed by Dr. Pomeranz at least 1 week prior to the scheduled date. The program coordinator or scheduling coordinator can help you find a time to present either within the didactic calendar or a non-Tuesday.
Ice Fishing 2025



2024 FMEC

2024 FMEC







Bethany Picker, M.D. (She/Hers)
Program Director
Women’s Health
Faculty
PickerBe@cmhc.org
Medical School: University of Cincinnati College of Medicine
Residency: University of Colorado Rose Family Medicine
Fellowship: Duke University Faculty Development
What I like most about working with medical learners is the privilege and honor of watching learners develop their competence, their style, and their identities as physicians. It is an amazing journey that residents take and to be part of it feels like such a gift. Residents consistently question both “how” and “why” we do things (both clinical care and curriculum) which drives reflection and innovation. I cannot imagine a more dynamic aspect of medicine.
My husband and I have raised our two daughters in Maine and continue to enjoy the woods, the water, and the wonder. We have two dogs who bring their own brand of crazy to our family. In addition to the typical outdoor Maine adventures, I play French Horn in a community band.
Clinical Areas of Interest: I always find it difficult to state my clinical area of interest. I started as a rural family physician doing inpatient, outpatient, OB and house calls and even though I have been teaching for a long time, that breadth of care has influenced my clinical identity.
Scholarly Work: Presentations at Residency Leadership Summit:
Sprint to Improvement (2022)
Leadership
Council on Academic Family Medicine, AFMRD Representative CAFM
Physician Leadership Accelerator Program
Starfield Summit Representative for Rural Residencies
National Innovation/Research Projects
Length of Training Study
Clinic First/FM Innovation in Continuity Clinical Experience

Annie Derthick, Ph.D. (She/Her)
Associate Academic Program Director
Director, Behavioral Science
Faculty
derthian@cmhc.org
Graduate School: University of Alaska
Area of Study: Clinical Community Psychology with a Rural and Indigenous emphasis
I fell in love with resident education when I completed my own clinical training in a residency clinic. There is no better place to do the work I want to do, which is to be engaged with the community to solve the problems that matter most. Primary care is the hub of community health and wellbeing in so many underserved communities, and residency clinics are perfectly situated to partner with patients, families, and communities to create innovative, lasting change. I consider it a privilege to educate family medicine residents. I love being a part of the journey of residents consolidating their identity as a family physician and agent of change in their community. My favorite moment is somewhere in the middle of third year when the picture finally comes into focus, and this learner, who I’ve been watching grow over the last couple of years, takes shape as the physician they were meant to be. They are confident, grounded, and ready to make a difference.
Outside of work, my absolute favorite thing in the entire world is my 7-year-old goldendoodle, Moxie. I have a 1-year-old poodle, Cricket, who is worming her way into my heart as well. I like to spend time with them, and my partner, Kris, outside in our backyard, especially in the fall. I love to read. And I love to laugh. Feel free to stop by any time if you have a good story to tell or want to hear one.
Clinical Areas of Interest: Integrated Behavioral Health, Supervision and Mentorship. Psychological Assessment, Motivational Interviewing, Health Behavior Change, and Structural Racism as a Social Determinant of Health.
Scholarly Work:
DISSERTATION
Derthick. A. O. The Sexist MESS: Development and initial validation of the Sexist Microaggressions Experiences and Stress Scale and the relationship of sexist microaggressions and women’s mental health (Doctoral dissertation). ProQuest Dissertations and Theses Global (No. 3470179).
BOOKS
David, E. J. R., & Derthick, A. O. (2017). The psychology of oppression. New York, NY: Sage.
PEER-REVIEWED JOURNAL ARTICLES
Brown, S. R., Friedman, R., McDermott, S., Oliveri, M., Derthick, A. O., & Picker, B. (2021). Highlights of the innovation showcase. Annals of Family Medicine, 19(4), 375-376. PMID#34264849

Genesis Juat, MD, Medical Director
Faculty
Juatge@cmhc.org
I have a deep-seated belief that everyone should have access to healthcare—it’s a right, not a privilege. And having primary care as the heart of it all is vital for keeping our communities healthy and thriving.
My own curiosity has taken me on a journey through a variety of healthcare settings, from Federally Qualified Health Centers (FQHCs) as far west as Seattle to rural clinics in Maine, and eventually into leadership roles in hospital systems. These experiences have given me a broad perspective and allowed me to keep my practice diverse and dynamic. Moving into resident education felt like a natural step, sharing my experiences, and learning together as we adapt to the ever-changing world of medicine.
My interests include dermatology within primary care, behavioral health integration, international medicine, substance use disorder treatment, and the exciting ways technology enhances our practice. Yet, despite all the tech advancements, I still have a soft spot for my trusty old stethoscope from med school—it’s been with me through thick and thin.
My spouse is a local Mainer, and together we have 2 strong-willed kids and 2 Seattleite golden retrievers who have made an impressive transition from the urban sidewalks of Seattle to enjoying the open fields and cold Atlantic waters of Maine.
Medical School: A.U.A. College of Medicine
Residency: Central Maine Medical Center Family Medicine Residency

Patricia (Patty) Collins, D.O., OMM (She/Her/Hers)
Faculty
collinpa1@cmhc.org
Medical School: University of New England College of Osteopathic Medicine
Residency: Central Maine Medical Center Family Medicine Residency
After completing my residency and serving as chief resident at CMMC, I was excited to be staying on as faculty. The culture at the residency was one that strives towards growth and commitment to quality education and patient care. Being a faculty member has allowed me to continue to practice medicine across both the outpatient and inpatient settings while incorporating my passion for medical education and teaching. I love working alongside residents and medical students, I find myself not only teaching but learning from our learners. It is a privilege to be a part of their individual growth as physicians.
Outside of work, I enjoy spending time outdoors. My husband and I love to take our daughter and dog hiking. I also enjoy biking, cooking, and attempting to garden.
Clinical Areas of Interest:
Inpatient Medicine
Family Planning
Breastfeeding Medicine
Scholarly Work:
Optimizing Graduate Medical Education during Early Residency
Society of Teachers of Family Medicine Residency Faculty Fundamentals Certificate

Chris Decker, D.O., OMM, DAAMA, DABOIM (He/Him)
Director of Integrative Medicine
Faculty
deckerch1@cmhc.org
Medical School: Touro University California
Residency: Central Maine Medical Center Family Medicine Residency
Fellowship: Integrative Medicine University of Arizona/ Maine Medical Center
I love being in an environment of active learners as it keeps me engaged, up to date, and provides unique perspectives that I don’t think I would be as exposed to otherwise.
There is an excitement and zest that I find energizing and motivating.
As faculty, I like to stress both the technical side of being a doctor but more importantly the healer/ humanistic side to build therapeutic relationships and individually tailored plans based on a person’s cultural background and personal values.
Outside of medicine, I enjoy being active whether it being playing soccer, frisbee or going on a hike and spending time with my wife, son, and dog.
Clinical Areas of Interest: Addiction, Integrative, Acupuncture, Homeless Youth
Scholarly Work:
Review of Effectiveness of Psilocybin for Depression. Integrative Medicine. 2022
Integrative Approach to Long Covid Seminar at Family Medicine Education Consortium. 2022
Creator and instructor for Intro to Integrative Medicine Course at Maine College of Healthcare Professionals 2021

Thomas Hattan, M.D.
Board Certified Palliative Care Medicine
Faculty
hattanth@cmhc.org
Medical School: Saint Louis University School of Medicine
Residency: Madigan Army Medical Center, Internal Medicine
Fellowship: Geriatrics, VA Madigan Army Medical Center
At the age of twelve I decided that I would be a Doctor and not a history teacher; thankfully my career has allowed me to create a medical practice but also share the joys of teaching. I have worked with the community of Lewiston/Auburn and the family medicine residency to provide care for in area Nursing Homes and Assisted Livings. Sharing that work living space with teammates, medical students, residents, nurse practitioners, and colleagues: I am proud of the home-based collaborative care we provide. In my work with medical learners, I strive to provide a community-based perspective that stresses the natural processes of the life, aging, and dying; how medicine can interfere and aid in these processes.
Teaching, learning, growing, the open exchange of ideas and practice: working with a Geriatric Team to provide as safe and comfortable place as we can is a rich challenge.
I live with my wife Robin and three dogs in Yarmouth, Maine. Three adult children enrich our world with adventures and growth. Seasons, travel, walks, gardening, sitting by the fire with a novel, I am proud and blessed with Yarmouth’s warm comfort.
Clinical Areas of Interest: Geriatrics and Palliative Care medicine and teaching. Helping medical learners understand the necessity of self, their individual perspective and voice as it impacts their practice of medicine. Understand and improve my own practice and team skill set. Build a Geriatric Team at the Family Medicine Residency.
Scholarly Work: My practice is that of a clinical provider. I am proud that five medical learners that I have shared my practice with have furthered their Geriatric and Palliative Care practice and education and of all the students and graduates that enrich our community.

Hannah Kazal MD, ScM
Faculty
Fellowship: Addiction Medicine Fellowship, Maine Medical Center
Residency: Sutter Santa Rosa–UCSF Family Medicine Residency
Medical School: Warren Alpert Medical School of Brown University
Dual degree: M.D., Sc.M. (Master of Science in Population Medicine)
She graduated from Brown University Medical School with dual MD and Master of Science in Population Medicine degrees. Residency pulled her to the West Coast, where she graduated from Sutter Santa Rosa-UCSF Family Medicine Residency as an HIV specialist and CREATE (Continuing Reproductive Education for Advanced Training Efficacy) trainee with advanced reproductive health skills. Through residency as a third-year running the inpatient medicine, obstetrical, and outpatient services, she discovered her enthusiasm for medical education and decided to pursue an academic fellowship in Addiction Medicine.
Clinical Areas of Interest: She is passionate about dismantling health inequities and expanding access for marginalized populations such as those living with SUDs, HIV, unhoused communities, and carceral histories. She is an advocate for the integration of harm reduction into clinical care and enjoys providing education on this evidence-based practice to colleagues, medical trainees, and patients. As a Family Physician, Dr. Kazal maintains a broad practice in comprehensive reproductive health, HIV/HCV prevention/treatment, and procedures with general primary care of patients and families through peripartum, childhood, and aging, from the acute hospital to community settings.

Lauren Nadkarni, M.D., CAQSM (She/Her/Hers)
Assistant Regional Dean, UNECOM, Family Medicine Residency
Sports Medicine
Faculty
nadkarla@cmhc.org
Medical School: Tufts University School of Medicine
Residency: Maine Medical Center, Portland, ME
Fellowship: Sports Medicine, Maine Medical Center, Portland, ME
I believe in promoting health and supporting preventative care efforts through physical activity based on the belief that ‘exercise is medicine.’ I work with patients using shared decision-making to provide creative solutions to their unique healthcare needs.
I enjoy working with underrepresented populations, and when the opportunity to create a new sports medicine program within the residency appeared, I was excited to step into the role. I enjoy combining my interests in sports medicine, point of care ultrasound (POCUS), and public health in a teaching environment, and look forward to continuing to learn from and teach residents and medical students for years to come.
When I’m not working, I enjoy traveling and being active outdoors, hiking, playing sports, tending my vegetable garden, and spending time with my family and my dogs.
Clinical Areas of Interest: Sports medicine, adolescent medicine, collegiate health, pediatrics, preventive care
I organize and teach a bi-annual CMHC Point of Care Ultrasound (POCUS) course for the system.
BIBLIOGRAPHY
Nadkarni L, Haskins A, Holt C, Dexter W. Reduction of High School Ice Hockey
Injuries With Implementation of New Checking/Boarding Rules. Clin J Sport Med.
2021;31(6):e420-e424. doi:10.1097/JSM.0000000000000846
Book Chapters/Invited Reviews
Nadkarni, L, Gillespie, HM, & Dexter, WW. (2019). Anterior Shoulder Instability in
M.D. Miller, et. al (Eds.), Essential Orthopaedics, Second Edition.
Case Reports
Nadkarni, L, Quinn, K, & Gillespie, H. (May, 2019). Knee Pain – Swimming in
Dangerous Waters. Presented at: American College of Sports Medicine
(ACSM) Annual Meeting; Orlando, FL, USA
Published Abstracts:
Nadkarni, L, Dexter, W, Holt, C, & Haskins, A. (April 2019). High School Ice
Hockey Concussion Rates Reduced with Implementation of New
Checking/Boarding Rule. Presented at: American Medical Society for Sports
Medicine (AMSSM) Annual Meeting; Houston, TX, USA
Non-print Scholarship:
Conte, J, Nadkarni, L, Derthick, A, Lucas, J, & Corbett, I. (October 2020). It’s Not
All In Your Head. Family Medicine Education Consortium (FMEC) Annual
Meeting; virtual.

Paige Picard, D.O. (She/Her)
Adolescent and Collegiate Health, Lifestyle Medicine
Medical Director, Health Services at Bates College
picardpa1@cmhc.org
Medical School: Lake Erie College of Osteopathic Medicine (LECOM), Erie PA
Residency: Maine Medical Center Portland, ME
One of the reasons I went to medical school was to “stay in school” which I later realized was a passion for the pursuit of knowledge and lifelong learning. I love that through academic medicine I can learn and teach individuals with varying skill levels from medical students to seasoned colleagues. One of my primary clinical interests is in lifestyle medicine, with a focus on preventing and reversing chronic disease through holistic approaches. Through my clinical work at Bates College, I now have the opportunity to grow, learn, share, and teach with college students and college administration. When not immersed in academia, I live just 30 minutes from Lewiston on a small tree farm with my husband and 4 children. We spend our time managing a wood lot, tending to a small garden, keeping bees, and cooking from scratch.
Scholarly Work: I am focused on lectures and presentations which have included both National and State annual conferences at Family Medicine Education Consortium (FMEC), Maine Osteopathic Association (MOA). I also serve on the Raising Readers Committee, a group dedicated to providing books free of charge at every well child visit from age birth to 5.

Jerry Pomeranz M.D. (Him/His)
Faculty
Jerome.Pomeranz@cmhc.org
Medical School: Frank H. Netter School of Medicine at Quinnipiac University
Residency: Memorial Hospital of South Bend
I chose to work in resident education because teaching the next generation of family medicine doctors is incredibly meaningful to me and multiplies my impact as a physician. What I like most about working with medical learners is the different perspectives they bring to the table, and the joy they experience when they learn a new skill. What excites me about the clinical learning environment is there is always new ideas to discuss. There are also so much flexibility in how to practice medicine in that setting. When I’m not at work you can find me at the disc golf course, playing my harmonica, listening to country music, and spending time with my family near Boston.
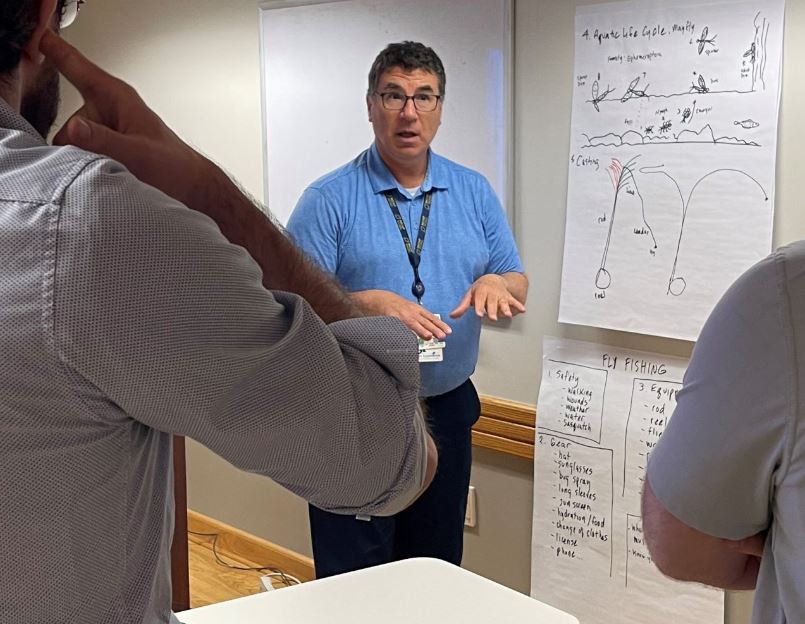
Clinical Areas of Interest: Wilderness/International Medicine, Obstetrics, Point-of-Care Ultrasound, Mental Health, and Procedures.
Scholarly Work: Baliunas, A.J., Pomeranz, J.E., & Zimmer, D.F. (2021, December). Vasculitis after COVID-19 Vaccination. Emergency Physician Monthly. Retrieved January 31, 2022, from https://epmonthly.com/article/vasculitis-after-covid-19-vaccination/.

Heidi Walls, M.D. (She/Her/Hers)
Sports Medicine
Faculty
wallshe1@cmhc.org
Medical School: Tufts University School of Medicine
Residency: Maine Medical Center
Fellowship: Sports Medicine, Maine Medical Center
A career in medicine is inevitably a commitment to lifelong learning, which totally excites me. The academic environment and the opportunity to educate the next generation of doctors truly fosters that growth. It’s a privilege to share my knowledge with our residents, and I get to learn from them as well. Working at the Central Maine Family Medicine Residency is just the best.
When I’m not working, I find joy in movement and the outdoors. If I didn’t choose a career in medicine, I would have become a carpenter or a coach.
Clinical areas of interest: Sports medicine, ultrasound, metabolic health, and conditions of the female athlete
CMMC Family Medicine Residency
76 High Street
Lewiston, ME 04240
Tel. 207-795-2184
Fax. 207-795-2190
The Nurse Residency Program at Central Maine Healthcare is a formal education program designed to extend the graduate nurse’s basic nurse education and skills and support them in the transition to professional nurse throughout a 12-month program. All nurses entering Central Maine Healthcare with less than one year of experience will be enrolled in the Nurse Residency Program, including all Registered Nurses and Licensed Practical Nurses.
The residency focuses on providing a culture that prioritizes and supports professional growth and learning. Our nurse residents are the future of healthcare in our community, so it is essential to provide them with the tools, training, and support they need for their success as they begin a new career.
The 12-month program consists of a standardized orientation comprised of organizational onboarding, skill acquisition rotations, regularly scheduled Professional Development Sessions, and frequent check-in with the Residency Program staff. Our goal is to integrate new nurses into our team while giving them the confidence, support, and education to succeed in their careers.
The Nurse Residency Program is a proven, evidence-based curriculum designed by Vizient and the American Association of Colleges of Nursing (AACN). We provide a one-on-one clinical experience with preceptors and ongoing support from experienced mentors, educators, and leadership. Initial structured skill acquisition education in the clinical setting supports the transition to practice based on quality safety initiatives. In addition, the residency provides foundational learning experiences and builds confidence before caring for a patient assignment.
Throughout the 12-month program, we offer multidisciplinary year-round integration of professional development sessions focused on enhancing clinical thinking, clinical judgment, skill development, knowledge application, and professional growth. Providing professional development strengthens commitment to nursing as a professional career as a life-long learner.
As part of the residency, we support evidence-based practice through an evidence-based project. Research shows that evidence-based practice directly links practice outcomes and care provided to improve health outcomes and reduce variation in patient care.
Go to Careers – myworkdayjobs.com and complete a New Graduate Nurse (RN) application
Angela Butler BSN, RN
Nurse Residency Program Coordinator
Central Maine Medical Center
207-330-7250
NurseResidencyProgram@cmhc.org
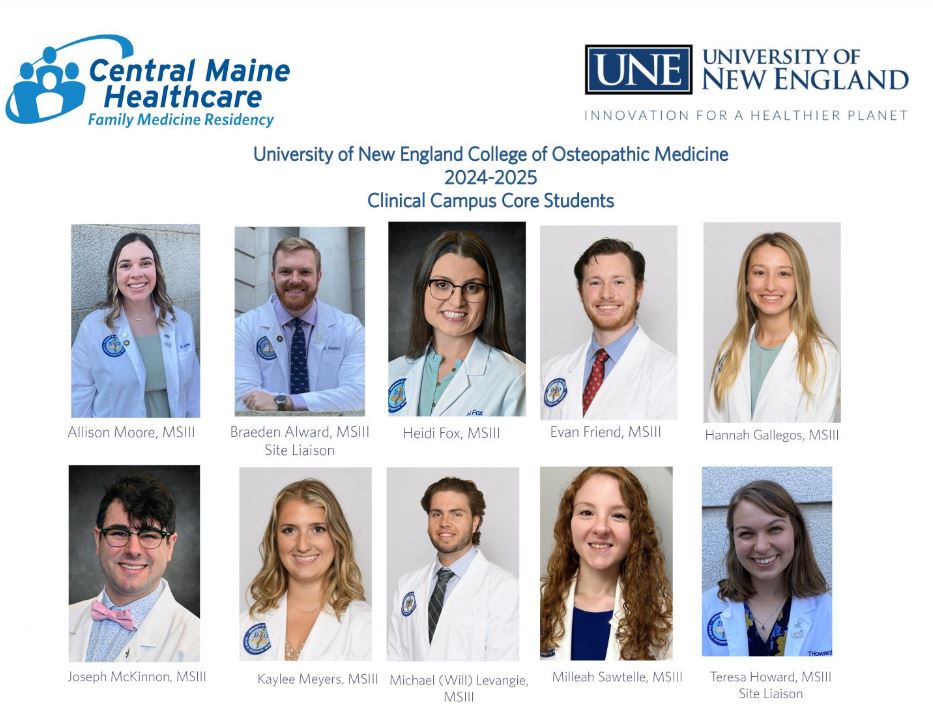
Central Maine Medical Center Family Medicine Residency provides clinical and educational experiences to third-year core students and fourth-year elective students. We are a very competitive site for clinical rotations. We strive to show compassion and respect to all and pride ourselves to immerse our students in vast clinical environment and a great experience. We advise applicants to apply months in advance in order to secure an approved rotation.
Our residency is a host Core Clerkship site for the entire third year of clinical experiences for the University of New England College of Osteopathic Medicine (UNECOM). We accept a total of twelve students from UNECOM, who are matched to our site through a lottery process.
We also are a core site for the following 3rd-year Family Medicine Clerkships:
We strive to provide an optimal learning experience by allowing students to be involved in all aspects of medical education. We will only schedule rotations when there is no conflict with resident education. Rotations are available to students from U.S., Canadian and offshore medical schools.
Documentation Requirements (once approved for a rotation):
What We Offer to Students:
Central Maine Medical Center Family Medicine Residency offers 3rd year student Core Clerkships to
The following elective clerkships are available at CMMC (clerkships are only scheduled when they will not conflict with resident education) and are coordinated by the Family Medicine Residency office. We only approve rotations that offer the most optimal education. We offer these rotations to students from U.S., Canadian and offshore medical schools.
Family Medicine (Sub-Internship)
We offer other rotations on a case-by-case basis. These specialties can include:
If there is a rotation you are interested in and did not see listed, feel free to contact us to determine if it might be something that can be arranged.
If you have questions regarding a clerkship, contact Mary Dooley at mary.dooley@cmhc.org
Central Maine Medical Center Family Medicine Residency provides clinical and educational experiences to third-year core students and fourth-year elective students. We are a very competitive site for clinical rotations. We advise applicants to apply months in advance in order to secure an approved rotation.
Our residency is a host Core Clerkship site for the entire third year of clinical experiences for the University of New England College of Osteopathic Medicine (UNECOM). We accept a total of Twelve students from UNECOM, who are matched to our site through a lottery process.
We also are a core site for the following 3rd-year Family Medicine Clerkships:
We strive to provide an optimal learning experience by allowing students to be involved in all aspects of medical education. We will only schedule rotations when there is no conflict with resident education. Rotations are available to students from U.S., Canadian and offshore medical schools.
Documentation Requirements (once approved for a rotation):
What We Offer to Students:
Program Director
Faculty
Presentations at Residency Leadership Summit:
Sprint to Improvement (2022)
PEP talks for All (2021)
Faculty
Program Director
Leadership
Council on Academic Family Medicine, AFMRD Representative CAFM
Physician Leadership Accelerator Program
Starfield Summit Representative for Rural Residencies Starfield Summit
National Innovation/Research Projects
Length of Training Study
Clinic First/FM Innovation in Continuity Clinical Experience
Associate Program Director, Inpatient Medicine Services and Curriculum
Faculty
“Faculty Development Needs Assessment”
Poster Presentation, Society for Teachers of Family Medicine National
Conference
“CCC on a mission: Developing a mission statement to add clarity, purpose, and
transparency”
Family Medicine Education Consortium
“In Touch with Inpatient Care: Osteopathic Principles and Practices in the Inpatient
Setting”
Family Medicine Education Consortium
Associate Academic Program Director and Director Behavioral Science
Faculty
DISSERTATION
Derthick. A. O. The Sexist MESS: Development and initial validation of the Sexist Microaggressions Experiences and Stress Scale and the relationship of sexist microaggressions and women’s mental health (Doctoral dissertation). ProQuest Dissertations and Theses Global (No. 3470179).
BOOKS
David, E. J. R., & Derthick, A. O. (2017). The psychology of oppression. New York, NY: Sage.
PEER-REVIEWED JOURNAL ARTICLES
Brown, S. R., Friedman, R., McDermott, S., Oliveri, M., Derthick, A. O., & Picker, B. (2021). Highlights of the innovation showcase. Annals of Family Medicine, 19(4), 375-376. PMID#34264849
Kam-Magruder, J., LeSage, K., Derthick, A.O., & Ackerman, L. (2018). An interprofessional residency curriculum in geriatrics and palliative care: PRiMER: Peer Reviewed Reports in Medical Education, 2(21). doi:10.2245/PRiMER.2018.183282
Derthick. A. O., Swift, J. K., Thompkins, K. (2018). A test of the utility of therapists’ and clients’ expectations in predicting treatment duration and outcomes. Journal of Clinical Psychology.
Swift, J. K., & Derthick, A. O. (2013). Increasing hope by addressing clients’ outcome expectations. Psychotherapy, 50, 284-287. doi:10.1037/aoo31941
Wong, G., Derthick, A. O., David, E. J. R., Saw, A., & Okazaki, S. (2013). The what, the why, and the how: A critical review of racial microaggressions research. Race and Social Problems, 6(2), 181- 200.
NATIONAL SERVICE:
Editorial Board, Family Medicine
Medical Editing Fellowship, STFM
Director Rumford Community Home
Faculty
FM Education Consortium, 2022 Post Covid Care: Integrative approach,
(Boutaugh, Decker and Picker)
CMMC CME Committee and CMMC FMR M&M Advisor
Boutaugh N, Derthick A. Creole Son. Fam Med. 2021;53(3):230-231.
https://doi.org/10.22454/FamMed.2021.485263.
Nicole S. Boutaugh, D.O. and Claudia K. Geyer, M.D. Intermediate Care Unit Implementation Impact on Medical Unit Rapid Response Team and Code Call Frequency. Maine Chapter Society of Hospital Medicine Poster Competition, Portland, ME May 2017
Faculty
Optimizing Graduate Medical Education during Early Residency
Society of Teachers of Family Medicine Residency Faculty Fundamentals Certificate
Director of Integrative Medicine
Faculty
Review of Effectiveness of Psilocybin for Depression. Integrative Medicine. 2022
Integrative Approach to Long Covid Seminar at Family Medicine Education Consortium. 2022
Creator and instructor for Intro to Integrative Medicine Course at Maine College of Healthcare Professionals 2021
Director of Osteopathic Education
Faculty
Lecturing at the Maine Osteopathic Associations semiannual conference
Lecturing for NEOMEN’s semi-annual OMM updates
Peer review published book review in STFM
Working on Lifestyle Medicine Board Certification
Assistant Regional Dean, UNECOM, Family Medicine Residency
Faculty
BIBLIOGRAPHY
Nadkarni L, Haskins A, Holt C, Dexter W. Reduction of High School Ice Hockey
Injuries With Implementation of New Checking/Boarding Rules. Clin J Sport Med.
2021;31(6):e420-e424. doi:10.1097/JSM.0000000000000846
Book Chapters/Invited Reviews
Nadkarni, L, Gillespie, HM, & Dexter, WW. (2019). Anterior Shoulder Instability in
M.D. Miller, et. al (Eds.),Essential Orthopaedics, Second Edition.
Case Reports
Nadkarni, L, Quinn, K, & Gillespie, H. (May, 2019). Knee Pain – Swimming in
Dangerous Waters. Presented at: American College of Sports Medicine
(ACSM) Annual Meeting; Orlando, FL, USA
Nadkarni, L, Bigosinski, K, & Gillespie, H. (April, 2019). Hit to the Head and Heck –
Shock to the Shoulders Presented at: American Medical Society for Sports
Medicine (AMSSM) Annual Meeting; Houston, TX, USA
Theses/Dissertation:
Tissue Engineering Approaches for Dentinogenic Restoration (2009). Advisor:
Dr. David Kaplan. Tufts University
Published Abstracts:
Nadkarni, L, Dexter, W, Holt, C, & Haskins, A. (April, 2019). High School Ice
Hockey Concussion Rates Reduced with Implementation of New
Checking/Boarding Rule. Presented at: American Medical Society for Sports
Medicine (AMSSM) Annual Meeting; Houston, TX, USA
Nadkarni, L, Dexter, W, Holt, C, & Haskins, A. (April, 2018). Reduction of High
School Ice Hockey Injuries with Implementation of New Checking/Boarding
Rule. Presented at: American Medical Society for Sports Medicine (AMSSM)
Annual Meeting; Orlando, FL, USA
Non-print Scholarship:
Conte, J, Nadkarni, L, Derthick, A, Lucas, J, & Corbett, I. (October 2020). It’s Not
All In Your Head. Family Medicine Education Consortium (FMEC) Annual
Meeting; virtual.
Faculty
Baliunas, A.J., Pomeranz, J.E., & Zimmer, D.F. (2021, December). Vasculitis after
COVID-19 Vaccination. Emergency Physician Monthly. Retrieved January 31,
2022, from https://epmonthly.com/article/vasculitis-after-covid-18-vaccination/.
White, D.A., & Pomeranz, J.E. (2018, July). Validity of consumer-marketed handheld
near infrared spectrometer.
Poster presented at AAFP National Conference, Kansas City, MO
CMMC FMR can support residents in most any area of interest, but based on our faculty areas of expertise, current clinical services, and community partnerships, there are some specific strengths of the program that include:
For residents interested in a career in teaching or doing scholarly work, they work on developing those skills and portfolio during residency. Several residents have completed an Academic Medicine elective rotation in the past, which has included partnering with faculty on a research project, spending additional time in our med student clinic, junior precepting, didactic teaching, completing peer-reviews, and presenting at conferences.
We provide a robust MOUD program for patients, and residents participate in all aspects of care including our low barrier bridge clinic and weekly support group as well as managing their own panel of patients on MOUD. For residents who would like additional training in Addiction Medicine, there are opportunities to spend additional time in these clinics, as well as work one-on-one with our Licensed Alcohol and Drug Counselor, who conducts Addiction Assessments of patients in early stages of recovery, and rotate with a community partner for inpatient experience.
Many of our residents have a passion for being agents of change in the community. Advocacy is a powerful way to use your voice as a physician to shape the landscape of health care, particularly at a local level, and residency is a great place to learn those skills. Several residents have completed an advocacy elective that has included speaking at the state legislatures, writing op-eds for the local newspaper, interviewing local and state representatives, researching health policy, and completing advocacy training.
The goal of the Selective is to provide a more compact and comprehensive exposure to the many venues which provide care for the frail elderly: the home, the clinic, assisted living communities, long term care, hospital-based palliative care, and community-based and inpatient Hospice Care. The frail elderly is a fast growing and underserved population which requires a unique set of clinical skills. The goal of this Selective is to help you to be confident and competent caring for elders in your practice after residency.
The Hospitalist in Family Medicine is designed to give residents a concentrated exposure to Hospital Medicine as it evolves into an exclusive area of practice. The resident will work directly with a hospital-based provider group and will participate in the care of patients in that environment. The resident is encouraged to explore all areas in which Hospitalists function which could also include opportunities to rotate in Bridgton or Rumford Hospitals. There may be opportunities to work on the Palliative Care Service as well as serve as a medicine consultant for patients admitted by other providers in the system. This experience may prepare the resident to apply for our or another Hospitalist fellowship.
The goal of the selective is to introduce residents to offering health care through an integrative medicine model. Integrative Medicine combines evidenced-based traditional western or allopathic and osteopathic medicine with other healing traditions, to create an individualized approach for the patient and to support the wellness of the health care provider and team. The resident will gain exposure to a variety of alternative health care providers via an experiential approach and learn to design a holistic method of practice for you and your patients.
Each resident completing the Integrative Medicine selective will also have the opportunity to participate with residents around the nation in the web-based Integrative Medicine in Residency (IMR) program designed by the University of Arizona. IMR is an in-depth competency-based curriculum in integrative medicine to be completed during the second two years of your residency. The IMR incorporates program and topic-specific exercises that residents can incorporate into their day-to-day family medicine experience. Arizona Center for Integrative Medicine
The resident in a sports medicine will have additional training in sports medicine, including opportunities for sideline game coverage, sports medicine research, and increased time in the sports medicine clinic, which allows for increased training in diagnosis and management of musculoskeletal issues. Residents have the opportunity to improve their skills with various procedures including musculoskeletal ultrasound, casting and splinting, joint injections and aspirations, and musculoskeletal x-ray interpretation. After completing this time in sports medicine, the resident should have increased competence at triaging and managing non-operative fractures, tendinopathies and other traumatic injuries, and be comfortable managing non-traumatic musculoskeletal complaints as well.

osteopathicrecognitioninformationbrochure.pdf
Program Goals: Through a variety of innovative curricular experiences integrated throughout the three years of residency (see below), Designated Osteopathic residents in our Family Medicine Program will have a unique and specific set of knowledge and skills with distinct behavioral, philosophical and procedural aspects related to the four tenets of Osteopathic medicine:
This will make you a highly skilled primary care physician capable of approaching patients with in-depth knowledge of Osteopathic Principles and strong skills-based approaches to acute and chronic medical conditions.
Logistics: Prior to entering as a designated Osteopathic resident, applicants should have sufficient exposure to osteopathic philosophy and the techniques of Osteopathic Manipulative Treatment (OMT). Educational background should include, but is not limited to: osteopathic philosophy, history, terminology, and code of ethics; anatomy and physiology related to osteopathic medicine; indications, contraindications, and safety issues associated with the use of OMT; palpatory diagnosis, osteopathic structural examination, and OMT. This could be satisfied by graduating from an Osteopathic Medical School.
If an allopathically trained resident expresses interest in Osteopathic Recognition (OR) they will have access to an equivalent of 200 training hours in Osteopathic Principles and Practice during their three years with us. Acceptance of residents into the ORT will be at the Director of Osteopathic Education’s discretion.
OMM Clinic: Designated Osteopathic Residents will be assigned to OMM clinic every month. Patients will be scheduled for 40 minutes. Initial visit will include history, osteopathic structural exam and appropriate focused physical exam, discussion of treatment plan with the attending physician and treatment with OMT (Osteopathic Manipulative Treatment). Residents are encouraged to treat their patients in continuity clinic. ACGME has requirements on attaining patient encounter numbers we will discuss with you.
Didactic Presentations: Designated Osteopathic Residents will be expected to complete the following:
While on inpatient and subspecialty services, designated Osteopathic residents may be asked to present one or more patients with a complete Osteopathic assessment and treatment plan.
Q. How does the Osteopathic Recognition complement the other required residency rotations? Does this training take the place of other rotations?
A. This is a longitudinal curriculum. Residents learn the additional educational material gradually over all 3 years and the information is integrated into a variety of the core family medicine rotations. Designated Osteopathic residents are given time during selected rotations to learn about additional Osteopathic approaches relevant to primary care. Monthly OMM didactics and semi-annual conferences allow residents to dedicate time to learning hands-on skills from OMM specialists. Designated Osteopathic residents still complete all the same residency rotations as their peers. The goal, first and foremost, is to produce well-trained and highly skilled family physicians; Osteopathic recognition offers the opportunity to apply additional knowledge in OPP and Osteopathic Manipulative Medicine to the benefit of all patients.
Q. What are the educational requirements of Designated Osteopathic Residents?
A. Participate in assigned activities including didactic sessions, noon and quarterly conferences, assigned OMT clinics, didactic presentation assignments, subspecialty clinics and inpatient assignments.
Q. How much time will the program take to complete?
A. The curriculum is longitudinal over 3 years of your family medicine residency. MD residents may need to set aside one of the available PGY2/PGY3 elective months for additional training activities.
Q. How do I apply? Is there a separate match application?
A. There is not a separate match application for this track. Residents interested in pursuing this track follow all the usual residency applications procedures and when you arrange your interview, indicate that you have an interest in hearing more about the Osteopathic Recognition. You will have the opportunity to ask more questions about the track during your interview and can tell us at that time if you’d like to be considered for the track.
Q. Who are the CMMC FMR faculty with training in Osteopathic Medicine?
A. Patricia Collins, D.O.
Paige Picard, D.O.
Christopher Decker, D.O.
Margo Goodman, D.O.
The Family Medicine Residency at Central Maine Medical Center will graduate residents who are:
As the Sponsoring Institution, Central Maine Medical Center commits to fostering a high-quality, safe, and trustful clinical learning environment. We provide residents and fellows access to cutting-edge, comprehensive, compassionate, and culturally responsive educational programming. Our team members promote professional identity development, emphasizing the importance of life-long learning skills and preparing skilled, ethical, innovative physicians who view themselves as agents of change in their communities and have the skills to practice in the rapidly evolving landscape of modern health care.
Given that time is limited during your interview day, below is a list of questions and answers about our residency that we hope will provide helpful information.
| Q | How long has CMMC been training Family Medicine residents? |
|---|---|
| A | Our program began in 1978 |
| Q | Where do your graduates practice Family Medicine? |
| A | Our goal is to train family physicians who are prepared to go to any community and be responsive to local needs, to be leaders, and agents of change wherever they land. However, we always hope they will choose to stay here. Many of our residents do choose to remain in Maine and Northern New England, working in ambulatory primary care and as hospitalists, some go on to fellowships such as Sports Medicine, Geriatrics/Palliative Care, and Addictions Medicine, and some take what they have learned and travel all across the globe to places such as Norway and New Zealand. |
| Q | What does “Clinic First” mean, and how would it influence my education? |
| A | Clinic First is a response to the reality that many family medicine faculty and residents only spend 1-3 half days per week in clinic, which is disruptive to continuity, access, and team-based care—many of the things that bring residents to family medicine in the first place. Residencies that are part of the Clinic First Collaborative make these essential elements of patient care and resident education a priority. At CMMC FMR, we have created a 2×2 block schedule, meaning residents are in clinic for 2 weeks at a time and then on rotation for 2 weeks at a time—no rushing off to clinic for a half day here and there in the midst of a busy rotation schedule. Wherever you are scheduled to be, you can fully immerse yourself in that learning experience. You always know when you will be in clinic, so you can plan ahead for continuity with your patients. |
| Q | What are some highlights of your Family Medicine Center, where I would see my continuity patients? |
| A | We serve a diverse cross-section of the Lewiston-Auburn and surrounding communities that includes elements of both urban and rural low-resourced communities. On any given day, you may see an unsheltered young person, a New Mainer (refugee) who has just arrived in the community, someone living “off the grid” in one of the surrounding rural communities, and an older Mainer, who has lived in the community forever. To meet the needs of our patients, we work as an integrated care team, which includes behavioral health. We provide interprofessional visits, where patients are seen by resident physicians, behavioral health, and pharmacy, for example, and we have monthly teamlet meetings to facilitate communication. Any member of the team can request an interdisciplinary team meeting (IDT) at any time to discuss a patient and develop a shared treatment plan. We also offer home visits that often include both a physician and behavioral health. One area we have been growing over the last few years, in direct response to the needs of our community is Addiction Medicine. We offer a Low Barrier Bridge clinic for OUD and several longer-term treatment pathways. |
| Q | What would my osteopathic education look like if I am a D.O.? |
| A | Our program is accredited under the ACGME with Osteopathic Recognition. All residents will have exposure to and education in osteopathic principles and practice. Osteopathic focused residents, which can include Allopaths, will have additional time practicing OMT in their continuity clinic and on the inpatient service. In addition, we offer osteopathic electives and an OMNN 2 for those looking for opportunities to advance their skills. We have 3 Osteopathic faculty, as well as several community Osteopathic Preceptors to support education and training. |
| Q | Do you have any focus on Resident Wellness as part of your residency program? |
| A | Yes. We have several wellness activities and initiatives including 5th Tuesdays (every 5th Tuesday afternoon the residents have an off-site resident-only gathering), monthly all-staff after work events, a wellness committee (Thrive), and 2 annual resident retreats. However, we believe that true wellness is maintained by residency culture, so we put most of our effort into building and nurturing a culture in our program where residents feel encouraged to bring their whole self to work, where they are supported in staying connected to those parts of themselves that exist outside of medicine, and where they are challenged to reflect on their meaning and purpose, so they grow as much as a person as a physician during their time in the program. |
| Q | What are the academic strengths that will benefit me if I train at CMMC? |
| A | Rigorous hospital medicine training, extensive exposure to Addiction Medicine, ongoing collaboration with a highly skilled Behavioral Health team, OMM, Integrative Medicine, Community-Engaged Learning, and Sports Medicine. Residents are also encouraged to develop autonomy and leadership from Day 1 of residency. They are first responders to Codes; they independently run the hospital service in PGY-2 and oversee interns in PGY-3; they take progressive leadership of their teamlet in clinic; and they are expected to participate in hospital-based committees with support from faculty. |
| Q | What would CMMC FMR offer to me as perks or value-added benefits? |
| A | Full benefits package, complimentary Health and Fitness Center visits including most classes, food stipends when on call, free parking. |
| Q | What is orientation like for new interns? |
| A | Orientation is a month-long experience that includes Continuity Clinic in the FMC; Orientation to the inpatient and outpatient EMR, orientation to the Hospital and the Lewiston-Auburn area; call done with a senior resident; BLS, ACLS and NRP courses with certification; meetings with the Program Director and your Academic Faculty Advocate; a series of new intern noontime didactics and an extensive introduction to competencies and your first rotation. |
| Q | What kinds of connections can I expect to make with the L-A (Lewiston-Auburn) community as a resident? |
| A | You will work in the Dempsey Challenge medical tent, United Way Agency fair, Community Service Day as part of intern orientation, a longitudinal 48-hour community project over the PGY II/III years and give talks in local schools. |
| Q | Can you tell me about the academic appointments and scholarly activities of the CMMC FMR faculty? |
| A | All residents complete a scholarly project, and there are many opportunities to be engaged in other research as well. See the Publications and Presentations section on the website for examples. |
| Q | Will I get to interact with and teach medical students? |
| A | Yes. We have 11 MSIIIs from UNECOM that complete their entire clerkship year in Lewiston. We also have FM clerkship students from Tufts and the University of Vermont and other medical schools. These students will work with you on inpatient and outpatient teams and you will have multiple opportunities to teach and guide their professional development. |
| Q | What is a WIMP? |
| A | The Wilderness and International Medicine Program is a special opportunity available to all residents at CMMC. Please check out our web page for more information. |
| Q | I have some special interests in Family Medicine – will I be able to tailor my education to assure that I gain competency in those areas? |
| A | Yes. We work very hard to individualize the education plan to meet each learner’s needs and desires. We have (An intensive education in a particular area that can include but is not limited to Children/Adolescent Care, Emergency Medicine, Geriatrics/Palliative Care, Inpatient FM Hospitalist, Integrative Medicine (formerly known as CAM), International Health, Maternity Care, Reproductive Health and Wilderness Medicine). We also have ample elective time during which you and your Academic Faculty Advocate can map out a plan to achieve your educational goals. |
