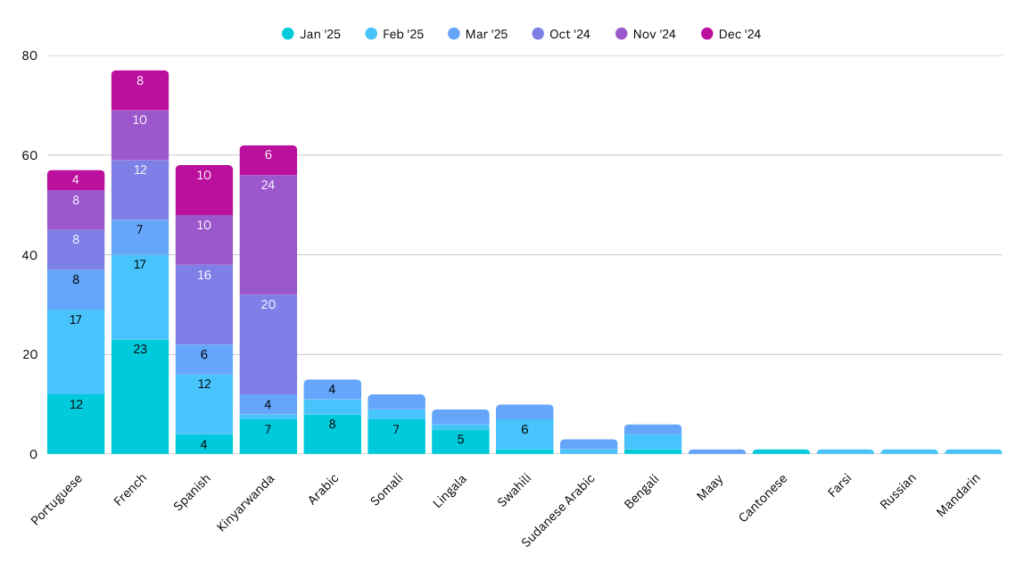
The following graph depicts the total number of calls received by our language assistance services program to overcome any patient/provider communication barriers. Our hope is to give insight to the diversity of languages spoken in our communities.
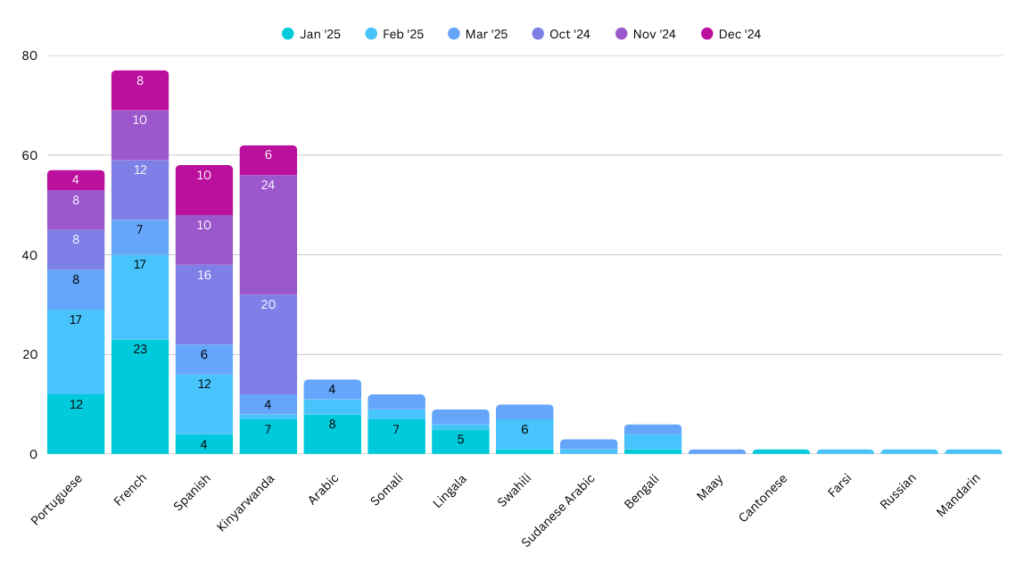
The following graph depicts the total number of calls received by our language assistance services program to overcome any patient/provider communication barriers. Our hope is to give insight to the diversity of languages spoken in our communities.
To apply for the fellowship, please email the following to Lori Lewis at lewislo@cmhc.org:
Once this information has been received your application will be considered complete and Mrs. Lewis or Dr. Stein will reach out to you.
Please contact Lori Lewis at lewislo@cmhc.org for further questions regarding the application process. With specific questions regarding the fellowship, you may email Dr. Stein at steinse1@cmhc.org. In addition, please see our listing on the SHM website 3
The following websites are available for further information:
Central Maine Medical Center
Central Maine Medical Center Family Medicine Residency and the hospitalists who make up CMH.
Visa sponsorship is unavailable.
References:
1Today’s Hospitalist May 2007 Iqbal, Yasmine Family Medicine Hospitalists: Separate and Unequal
2Supplement to The Journal of Hospital Medicine Jan/Feb 2006: The core competencies in Hospital Medicine: A Framework for Curriculum Development
3SHM Website
Central Maine Medical Center offers a competitive PGY-4 salary, in addition to the opportunity for loan repayment, to new hospitalist fellows.
The hospitalist fellow receives a full range of benefits, as well as four weeks of paid vacation. Also, $3,500 and one week of time are offered for continuing medical education. Additional monies are available for incentives such as extra shifts worked.

Bethany Picker, Residency Program Director
Undergraduate: Bryn Mawr College
Medical School: University of Cincinnati
Residency: University of Colorado, Rose Family Medicine
Fellowship: Faculty Development, Duke University
“I am from rural Connecticut which, despite what you may think, is not an oxymoron. As my brother likes to say, “The town’s population only broke 1000 when the New Yorkers came in the summer.” I loved it there and when I had to decide where to practice, I wanted a similar area. So, after residency I came east to Maine and practiced full scope family medicine in a rural area.
Then, I began teaching. It started with a student here and there—my practice was an AHEC site for students from the University of New England. Then I had a Nurse Practitioner from the University of Maine in Orono for a whole semester. I was bitten by the bug and wanted to make teaching a bigger part of my life.
Even though I had only been with my patients less than three years, it was hard to leave. I told them the adage I tell myself -“ If you want to feed someone for a day, catch a fish, if you want to feed someone forever, teach them how to fish.” I feel I am helping underserved patients everywhere by teaching residents and medical students. Now, being here with my husband and children, I love where we live and what I’m doing. What could be better?
CMMC Family Medicine Residency is simply a great place to work. I have colleagues that are smart, thoughtful, nice and fun. The residents are an energetic, inquisitive group that keep me on my toes. As Program Director, I have had the opportunity to work with the staff in new ways and have been equally impressed by their initiative and drive.
Lewiston itself is a nice mix of small city and small town. It is easy to get to the outdoor activities we love as well as a night out in Portland.
My medical interests have changed and grown recently. I am currently the program director and now have more interest in developing systems of care that treat patients effectively and efficiently. This includes patient safety, developing lasting effective patient relationships and ensuring high quality care. I enjoy thinking about and trying to influence healthcare policy on a national level. I continue to maintain my interest in women’s health including maternity care. I love caring for young families.”

Seth A. Stein, M.D., Director
Undergraduate: B.S., The Pennsylvania State University
Medical School: M.D., St. George’s University School of Medicine, Grenada, West Indies
Residencies: Family Medicine, Grant Medical Center Family Medicine Residency, Columbus, Ohio; Chief Resident, Family Medicine, Grant Medical Center, Columbus, Ohio.
Fellowships: Central Maine Medical Center Hospital Medicine Fellowship, Lewiston, Maine. Graduated 2016
Dr. Stein is residency trained and board-certified in family medicine. He has practiced as a hospitalist since completing his fellowship in 2016. Additionally, he has a Designation of Focused Practice in Hospital Medicine through the American Board of Internal Medicine.
Dr. Stein has been with the Central Maine Medical Center Hospitalist Group since 2015. In addition to being a Hospitalist, Dr. Stein is the former Director of the Inpatient Medicine Teaching service for the Family Medicine Residency program at Central Maine Medical Center. He continues to be engaged in numerous quality, safety and process improvement efforts at Central Maine Healthcare, and is a member of the Graduate Medical Education Committee. He continues to be passionate about teaching and to further this interest he has taken on the role as Director of the Central Maine Medical Center Hospital Medicine Fellowship in 2022.

Dr. Kyle Rattray
2020-2021 Fellow

Dr. Kaitlyn Losey
2018-2019 Fellow

Dr. Sophia Thomas
2017-2018 Fellow

Dr. Elizabeth Fleming
2017-2018 Fellow
Longitudinal Project: Reducing Mortality of Patients Admitted with Acute Exacerbation of Chronic Obstructive Pulmonary Disease Case study: Say Yes to the DRESS: Consider Rare Syndromes when Encountering a Patient with Rash. Organizer of multidisciplinary Chronic Obstructive Pulmonary Disease (COPD) work group to review the COPD care set, discuss evidence-based interventions, and determine how to best operationalize those interventions at our hospital. Ongoing resident and medical student education through regular preparation and presentation of case studies. Attendance at the National Society of Hospital Medicine meeting in Orlando, Florida and the annual meeting of the Maine chapter of the Society of Hospital Medicine. Longitudinal project presented at the meeting of the Maine chapter of the Society of Hospital Medicine, Portland, Maine, May 12, 2018. Volunteer at the Dempsey Challenge, Lewiston, Maine, in support of the Patrick Dempsey Center for Cancer Hope and Healing, 2017. Dr. Fleming completed a residency in Family Medicine and Community Health through the University of Minnesota in 2004. This was followed by work as the clinical director of an immigration detention center, experience in community health in South America and Haiti, and three years as a rural full-spectrum family physician. She joined the Central Maine Medical Center hospitalist team after her fellowship.

Dr. Daniel Matta
2016-2017 Fellow
Longitudinal Project: Reducing use and care variation of inappropriately prescribed IV anti-hypertensives, on-going. Clinical Vignette: Rapidly progressive renal disease: A deposition problem. Poster accepted and presented at Society of Hospital Medicine (SHM) Annual National Meeting, Las Vegas, NV 2017. Clinical Vignette: When “lockjaw” is the least of your concerns: A generalized spastic event. Poster accepted, presented and First Place winner at Society of Hospital Medicine (SHM) Maine Chapter Annual Meeting, 2017. Participant on multidisciplinary Heart Failure committee. Focus on the evaluation and optimization of heart failure treatment and disposition of admitted patients. Ongoing fellow, resident and medical student education including in-training examination preparation and fellow seminar organizer. Community preceptor for the Central Maine Medical Center Family Residency Program. Assistant Director, Hospital Medicine Fellowship 2017 – Present. 5K run participant, The Dempsey Challenge, Lewiston, ME in support of the Patrick Dempsey Center for Cancer Hope and Healing, 2016. Dr. Matta completed his fellowship training in 2017 and joined us after completion of his residency at Bayfront Family Medicine Residency in St. Petersburg, Florida. He is fully engaged as a member of our program and group as is evidenced by above accomplishments.

Dr. Kara Callahan
2016-2017 Fellow
Longitudinal Project: Quality Inter-Hospital Communication: A Novel Way to “Connect” Accepted for presentation and winner of Maine SHM Research, Innovations and Clinical Vignette Competition. When “lockjaw” is the least of your concerns: A generalized spastic event Society of Hospital Medicine (SHM) Annual National Meeting, National Harbor, MD. Longitudinal Project: Quality Inter-Hospital Communication: A Novel Way to “Connect” Participant on multidisciplinary Sepsis committee. Responsible for reviewing sepsis cases and hospital-wide adherence to Sepsis quality improvement initiatives. Participant in Hospital Based CEQS, CMMC- responsible for reviewing, discussing and initiating quality-based initiatives within the hospital. Dr. Callahan has joined as a faculty attending for the Family Medicine Residency program here at Central Maine Medical Center with an emphasis on resident education on the inpatient teaching service. She additionally serves as adjunct faculty for Tufts and Boston University School of medicine. She continues to work per diem with the hospitalist group.

Dr. Nicole Boutaugh
2016-2017 Fellow
Longitudinal Project: Intermediate Care Unit Implementation Impact on Medical Unit Rapid Response Team and Code Call Frequency Clinical Vignette: Unveiling a Rare Aorto-Atrial Fistula. Poster presented at Society of Hospital Medicine (SHM) Annual National Meeting, Las Vegas, NV May 2017.Participant on multidisciplinary Intermediate Care Unit committee. Focus on the implementation and evolution of a medical intermediate care unit and the subsequent impact on quality of patient care as well as hospital resource utilization. Participant on Infection and Prevention Regulatory Committee. Multidisciplinary team with focus on eliminating hospital associated infection. Resident and medical student educator on the Internal Medicine Teaching Service. Maine Chapter Society of Hospital Medicine Poster Competition Presentation: Intermediate Care Unit Implementation Impact on Medical Unit Rapid Response Team and Code Call Frequency. Grand Rounds: Morbidity and Mortality conference, Code Status: A Pivotal Decision March 2015. Dr. Boutaugh is one of our current Adult and Acute Rehabilitation Hospitalists, who joined us after completion of her residency at CMMC in Lewiston, ME. She is an active member of both the group and the local community.

Dr. Seth A. Stein
2015-2016 Fellow
Longitudinal Project: Impact of Palliative Care Consultation on Patients with Sepsis in the Intensive Care Unit Clinical Vignette: Fatal Disseminated Cryptococcal Infection in a HIV-Negative Patient. Poster accepted with planned presentation at Society of Hospital Medicine (SHM) Annual National Meeting, San Diego, CA 3/2016. Participant in multidisciplinary Sepsis committee. Focus on the evaluation of septic patients admitted to the ICU with palliative care consultation compared to patients without palliative care consultation. Retrospective chart review that will serve as a platform for future research endeavors. Accepted for presentation: Bariatric Surgery and the Role of the Family Physician: Maine American Academy of Family Physicians annual meeting, 4/2016. Ongoing resident and medical student education including in-training examination preparation. Anticipated attendance at national SHM meeting San Diego, CA and Maine Chapter SHM meeting. Grand Rounds: Morbidity and Mortality conference, Severe Lower Extremity Weakness 20155-10K run participant, The Dempsey Challenge, Lewiston, Maine in support of the Patrick Dempsey Center for Cancer Hope and Healing, 2015. Dr. Stein is one of our current fellows who joined us after completion of his residency at Grant in Ohio. He is fully engaged as a member of our program and group as is evidenced by above accomplishments.

Dr. Sara Sterling
2015-2016 Fellow
Longitudinal Project: Impact of assay change on inpatient Clostridium Difficile patients Clinical Vignette: Extensively Drug-Resistant Tuberculosis Extending Its Reach. Poster accepted with planned presentation at Society of Hospital Medicine (SHM) Annual National Meeting, San Diego, CA 3/2016. Participant on multidisciplinary Clostridium Difficile Committee – dedicated to developing and implementing strategies regarding reducing healthcare associated infections. Grand Rounds: Morbidity and Mortality conference, Severe Lower Extremity Weakness 2015. Ongoing resident and medical student education including clinic preceptor role. Anticipated attendance at national SHM meeting San Diego, CA and Maine Chapter SHM meeting Medical Volunteer, The Dempsey Challenge, Lewiston, ME in support of the Patrick Dempsey Center for Cancer Hope and Healing, 2015. Dr. Sterling is one of our current fellows. She joined us after residency at Geisinger in Pennsylvania and medical school here in Maine at the University of New England College of Osteopathic medicine. She is actively participating and contributing to our group and institutional culture.
Dr. Abraham Jacob
2014-2015 Fellow
Longitudinal Project: Mortality and Readmissions after Acute Stroke Clinical Vignette: Hemosuccus Pancreaticus: An Unusual Cause of GI Bleed. Poster presented at Society of Hospital Medicine (SHM) Annual National Meeting, National Harbor, MD 2015. Also presented above clinical vignette at Maine Chapter, Society of Hospital Medicine RIV competition 2014. Participated in Acute Neurology Care Committee reviewing mortality of patients with stroke before and after implementation of guideline-based care. Resident and medical student education and service attending role throughout the academic year. Dr. Jacob left the field of urgent care to enter the hospital medicine fellowship here at CMMC. He accepted and continues in a permanent nocturnist position with Catholic Medical Center in Manchester, NH.

Dr. Dena George
2013-2014 Fellow
Longitudinal Project: Cryptogenic Stroke Protocol: Enhancing Secondary Prevention of Stroke Presented Evidenced Based Management of Acute Stroke, Maine Academy of Family Medicine annual meeting, Portland, ME 2014. Presented clinical vignette; Hit with Clots after CABG, at Maine Chapter, Society of Hospital Medicine RIV competition 2014. Active participant, Acute Neurology Care Committee, focusing on reviewing and setting protocols for cryptogenic stroke. Provided extensive resident and medical student education including approximately 30 interactive sessions over the course of the year as well as inpatient service leadership. Dr. George joined the CMMC Hospital Medicine fellowship after honorable discharge from her career in the United States Army. Upon completion of her fellowship, Dr. George entered into the practice of adult hospital medicine with Sound physicians and is currently working at St. Joseph Regional Medical Center in Bryan, TX.

Dr. Talitha Sannes-Venhuizen
2013-2014 Fellow
Longitudinal Project: Inpatient Order-set with Decision Support for Accurate use of Novel Oral Anticoagulants Competition Winner, Innovation category of Maine Chapter, Society of Hospital Medicine RIV competition 2014, Novel Oral Anticoagulants: Standardized Practice Guidelines Led multidisciplinary team in design, approval and enactment of institution wide oral anticoagulant order sets with decision support. Provided extensive resident and medical student education as well as attending on the inpatient teaching service. After two years of hospitalist work, Dr. Sannes-Venhuizen pursued fellowship to enhance her ability to provide evidenced-based and procedural care in a rural setting. Upon successful completion of the fellowship, she returned to her native Minnesota and is working as a hospitalist in a variety of practice settings. She is also home schooling her children and providing home-based care to a local Amish population.

Dr. Swapna Gummadi
2012-2013 Fellow
Longitudinal project: Standardization and Improvement of Hip Fracture Management: A Multidisciplinary Approach Original Research: Employment Opportunities for Hospitalists Trained in Family Medicine, Gummadi, Geyer, Rossi, Journal of Hospital Medicine 9 Suppl 2 :17, poster presented, selected as finalist, SHM annual national meeting, Las Vegas 2014. Longitudinal project poster accepted and presented at Society of Teachers of Family Medicine annual national meeting 2013. Active member of Orthopedic Institute of Central Maine (OICM) Inpatient workgroup and Hip Fracture sub-group responsible for ongoing implementation, monitoring and education. Clinical Vignette: Blindness of the Heart: An Unusual Cause for Transient Bilateral Vision Loss accepted and published in the Journal of Hospital Medicine 8 Suppl 1:912, 2013. Poster accepted and presented in RIV competition at the Society of Hospital Medicine annual national meeting 2013. Dr. Gummadi accepted a permanent position with CMH and practices primary and consultative care of adult inpatients, serving as associate chief of the section of adult hospital medicine. She continues her work with OICM on improvement in the care of patients with hip fractures. She is active on the Peer Review committee and teaches residents, medical students, and fellows. Dr. Gummadi also sits on the board of the Maine Academy of Family Physicians with an interest in increasing resident involvement and promoting original research and presentation.

Dr. Mark Grohman
2012-2013 Fellow
Longitudinal Project: Novel Oral Anticoagulants: Provider Familiarity Compared with Prescribing Patterns Original Research: Novel Oral Anticoagulants: Provider Familiarity and accuracy of Use in Community Practice, Grohman, Geyer, accepted in the Journal of Hospital Medicine and poster presented at SHM annual national meeting, Las Vegas 2014. Presented project-related educational session on novel oral anticoagulants (NOAC’s) at the Maine academy of Family Physicians annual meeting 2013. Presented NOAC talk at Maine Society of Hospital Medicine chapter meeting 2013. Presented NOAC educational sessions at CMMC to multiple disciplines Clinical Vignette: Acute Ataxia with Negative Neuroimaging: Consider an Uncommon Polyneuropathy accepted and published in the Journal of Hospital Medicine 8 Suppl 1:801, 2013. Poster accepted and presented in RIV competition- honored with selection as finalist at the Society of Hospital Medicine annual national meeting 2013. Dr. Grohman accepted a position at Southern Maine Medical Center in the adult hospitalist program. He will be both the first hospitalist trained in family medicine as well as fellowship-trained physician in his group and will provide primary and consultative care of adults. He plans to continue his work with NOAC’s including education and improvements in patient care.

Dr. William Peternel
2011-2012 Fellow
Longitudinal Project: Impact of Pre-discharge Intervention on Post-discharge Accuracy of Medication Reconciliation: a Pilot Study Presented project results-which were consistent with recently published larger scale studies- and offered related education to CMH, CMFMR and institutionally at CMMC Presented project-related workshop entitled Care Transitions, a Hospitalist’s Perspective at the Maine Academy of Family Physicians annual meeting 2012, and at the New Hampshire Osteopathic Association Winter symposium 2013. Dr Peternel has started his own hospitalist company, New England Per Diem Hospitalist LLC. He provides services at various community facilities including continued work with CMH. He also continues his decade-long commitment to Veteran’s care and proudly serves in the United States Navy Reserve where he is assigned to Camp Pendleton Naval Hospital. In addition, he maintains a legal consulting business and runs a family farm, Rock Farm Natural Beef.

Dr. Carlos Villamarin
2010-2011 Fellow
Longitudinal Project: The Care of the Patient with Stroke. A multi-pronged institutional process improvement project including development of guideline-based order sets, their implementation and continued monitoring of use. Presented summary of work at CMMC rounds as well as at Acute Neurology Care Committee meetings. Poster accepted and presented at Society of Teachers of Family Medicine annual meeting 2011. Acute Neurology Care Committee and Reduction in Variation of Care for Stroke work group member. Longitudinal work an instrumental part in CMMC’s success at attaining first bronze, and now silver award recognition from Get With the Guidelines-Stroke. Dr. Villamarin has also joined CMH doing primary and consultative adult inpatient care and is currently an associate chief of the section of adult hospital medicine. In addition to his continued work on stroke care, Dr. Villamarin has been recognized for his teaching skills and continues to be involved in resident and fellow education. He has lead patient safety initiatives as well as a program to reduce provider paging and distraction.

Dr. Shauna McElrath
2009-2010 Fellow
Longitudinal Project: A Survey of Demographics, Employment Settings, and Scope of Practice of Hospitalists trained in Family Medicine Presented longitudinal research project at 2010 Maine Academy of Family Physicians annual meeting Poster accepted and presented at Society of Hospital Medicine 2011 annual meeting Publication of report describing results of project published in The Hospitalist, December 2010. Dr. McElrath is now practicing hospital medicine with CMH. Her work includes primary and consultative adult inpatient care, resident and fellow education, and an emphasis on palliative care medicine. She is board-certified in palliative care and is the medical director for Androscoggin Home Care and Hospice.
In 2009, Central Maine Hospitalists (CMH), in collaboration with Central Maine Family Medicine Residency (CMFMR), began offering a one-year fellowship for a family medicine or internal medicine graduate interested in pursuing a career as a hospitalist. Based on our highly successful initial experience with this program, in 2012 we expanded the program to include up to two fellows per academic year. We hope you will contact us if you are interested in focusing your career on inpatient medicine.
CMH was established with five experienced physicians in 2004 and has now grown to over thirty board-certified physicians and associate professional staff (NP/PA). We care for over 50% of the inpatient population at Central Maine Medical Center (CMMC), a 250-bed community teaching hospital as well as provide care at our affiliated critical access hospitals. All members of CMH are actively involved in a number of hospital processes including: division and group leadership, quality improvement, guideline development and implementation, patient safety, medical education, palliative care and information technology. We are also involved in the Society of Hospital Medicine (SHM), including Fellows and Senior Fellows of Hospital Medicine. Several of our members have earned a Recognition of Focused Practice in Hospital Medicine (RFPHM). Our group members have been active in and presented at SHM local chapter meetings, as well as national SHM forum leadership, committee membership and leadership. All members of the group are committed teachers involved in educating the hospitalist fellows, residents, medical and pharmacy students.
CMFMR has been educating family physicians since 1978. We provide care and training to diverse populations and our graduates are regularly hired into the hospital system. The opportunity to partner with the hospitalist group builds on our reputation for excellent inpatient training and our flexibility in establishing programs to meet student and resident needs. The department of family medicine has established a reputation for advanced thinking in organizing for the provision of care and has become a research setting for the rest of the outpatient practices at CMMC. Modeling excellence in interdepartmental cooperation, CMH and CMFMR are exceptionally well-suited to educating Hospitalists Trained in Family Medicine (HTFM).
Dr. Stein and our program were recently featured in The Hospitalist, August 2019: “We rely heavily on the Core Competencies in Hospital Medicine developed by SHM, which emphasize clinical conditions, medical procedures, and health care systems. Gaining fluency in the latter is really what makes hospital medicine unique,” Dr. Stein said. “Often residency graduates seeking work in hospital medicine are insufficiently prepared for hospital billing and coding, enacting safe transitions of care, providing palliative care, and understanding how to impact their health care systems for quality improvement, patient safety and the like,” he added.
Dr. Stein said his fellowship does not mean just being a poorly paid hospitalist for a year. “The fellows are clearly trainees, getting the full benefit of our supervision and supplemental training focused on enhanced clinical and procedural exposure, but also on academics, quality improvement, leadership, and efficiency,” he said. “All of our fellows join SHM, go to the Annual Conference, propose case studies, do longitudinal quality or safety projects, and learn the other aspects of hospital medicine not well-taught in residency. We train them to be highly functional hospitalists right out of the gate.”
