Symptoms of neurological disorders aren’t easy to navigate – neck pain, dizziness, blurred vision, tremors, and dozens more. They often resemble the symptoms of too many other ailments and can be hard to self-diagnose.
Enter the board-certified neuroscience team at Central Maine Healthcare, who are trained to diagnose and treat the full range of diseases linked to the brain, spine, muscles and nerves. By coupling cutting-edge technology with their compassionate care, our neurology team will take you in hand, identify your specific problem and design your personal treatment plan.
Back and Neck Pain
If you’re experiencing ongoing or severe back and neck pain, the neck and spine specialists at Central Maine will diagnose your problem and work with neurologists and other medical staff to find the source of your discomfort and create a treatment plan.
Why Your Back or Neck Hurts: With back-pain, your movements may be limited. You may even have a stiff neck, which makes it difficult to move your head from side to side. Back pain like this could be caused by something as simple as carrying a heavy bag on your shoulder.
Or your back pain may be a result of a more serious disorder like:
Herniated disc: When a disc protrudes in an abnormal way, it creates a hernia.
Spinal degeneration: Like all parts of the body, your spine can deteriorate over time, and you can lose your ability to walk and stand erect easily.
Spinal stenosis: The spaces within your spine can grow narrow, causing pressure on your nerves. Stenosis often is caused by arthritis and usually happens in your lower back or neck.
Chronic back pain: Once you’ve injured your back, if it’s not treated or doesn’t heal correctly you may experience pain over time.
Diagnosing and Treating Back and Neck Pain: Identifying the source of your pain usually starts with an X-ray to rule out injuries to bones or muscles. Your doctor also may order at CT or MRI scan to pinpoint the problem. You may also undergo an EMG (which is done via fine needles inserted into the muscles) to see whether certain nerves are working properly. A blood test is often added to check for inflammation or an infection. The treatment, of course, depends on the nature of your condition and always is personalized. Many patients respond well to a simple regimen of physical therapy, rest, exercise and medications. However, your individual program might include strength training and aquatic therapy or wearing a foam collar. From there, solutions get more sophisticated:
Baclofen Pump: With this advanced procedure, a small machine is implanted in your chest and delivers pain medication directly to your spinal cord.
Spinal Cord Stimulation Therapy: The stimulation happens in your brain. An electric current blocks your brain’s ability to sense pain in your spinal cord.
Surgery: More serious spine and neck conditions call for surgery, ranging from spinal fusions to vertebrae removal. Many procedures are computer-assisted or performed by robots, giving the surgeon a better view than they’d have in traditional operations, with more accurate results.
Regardless of why you’re feeling back or neck pain, CMH specialists can help get your relief.
Brain and Spinal Tumors
At Central Maine Healthcare, we focus on aggressively treating your tumor as soon as possible. Your treatment plan might include radiation, chemotherapy or surgery, and we will make sure you have the support to follow your personalized treatment.
Dementia
Dementia isn’t just one disease, it’s a group of symptoms that affect your memory, thinking and social abilities. Fortunately, at Central Maine Healthcare, you have some of the country’s best resources at your disposal, working quickly to diagnose dementia.
What Does Dementia Look Like? Dementia is tricky to diagnose because its symptoms can signal a long list of unrelated disorders. Some forms of dementia are progressive, like Alzheimer’s disease or Lewy Body dementia. But some types of dementia can be reversed. If it’s caused by an endocrine problem, such as a low-functioning thyroid or by dehydration or certain infections, the dementia stops when those conditions are addressed.
For most dementia, however, there is no cure — but modern treatments can treat the symptoms and slow the disease’s progression. Symptoms generally fall into two categories: cognitive and psychological.
Cognitive symptoms include:
- Memory loss
- Difficulty communicating
- Planning or organizing
- Confusion
Psychological symptoms include:
- Personality changes
- Depression
- Anxiety
- Paranoia
- Inappropriate behavior
How We Diagnose Your Dementia: Finding the reason for your dementia is a process. It involves a variety of cognitive and psychological tests. Your neurologist will work to reach an accurate diagnosis and design a treatment plan. In order to pinpoint your type of dementia, doctors will first look at your risk factors for dementia: your thorough health history, including your age and family illnesses. Then, they’ll look for signs of depression, diabetes, Down syndrome, sleep apnea, smoking or heavy alcohol use — all of which could influence dementia.
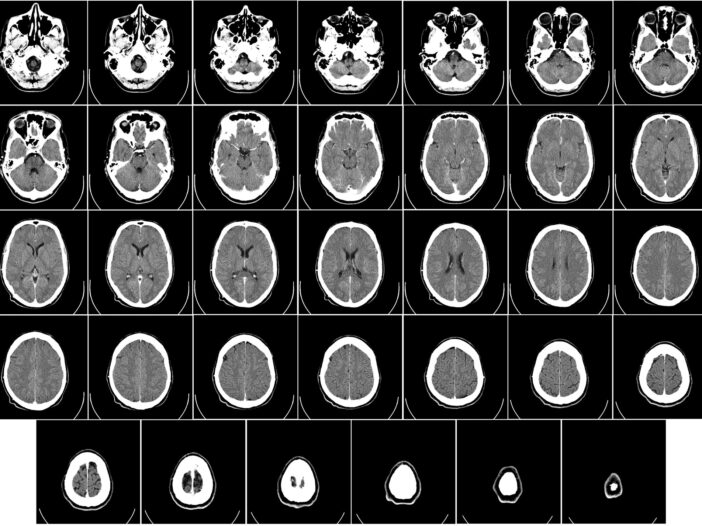
Our doctors will also test your memory, your language skills, your visual perception, and your ability to focus, reason and solve problems. They’re also likely to run CT and MRI scans to check for signs of stroke, tumors or bleeding in your brain. A PET scan can document your brain activity and tell doctors if the protein associated with Alzheimer’s (called amyloid) is present.
What We’ll Do for Your Dementia: Once we know exactly why you’re exhibiting symptoms, our physicians work on managing them. Almost always, they will prescribe medications to ease your symptoms. You’ll likely take a med such as Aricept — a cholinesterase inhibitor — that will boost your levels of the brain chemical that helps restore your memory and judgement skills. These medicines are common in treating Alzheimer’s, Parkinson’s and Lewy Body.
Other medicines regulate additional brain chemicals that affect your depression, ability to learn, and sleep. Beyond medications, we provide help that can improve your everyday life and independence:
Occupational therapy: Our therapists will teach you coping strategies, which can help you perform simple tasks such as laundry and making coffee. Their aim is to prevent falls and other accidents and prepare you for progression of the illness.
Modify your environment: Central Maine will do everything possible to make your home safer. We can help you reduce clutter and noise, hide items such as knives and car keys, and make sure you are visited regularly.
Modify your tasks: We’ll look at everything you do during the day and find ways to make those tasks easier. You’ll have structure and routine in your day, which will help you learn to focus on small successes.
Epilepsy
People with epilepsy can rarely predict when they’re about to have a seizure. The good news is that with Central Maine Healthcare’s help seizures can be controlled. Our highly trained experts successfully treat people with epilepsy every day. Epilepsy can develop at any age. For your own safety, if you or someone in your family has seizures, get help right away.
What Causes Seizures? We know that seizures are triggered by sudden changes in your brain’s electrical activity, but what causes those electrical surges? Seizures often start after a head injury. They might also begin after a stroke or when a tumor develops. During a seizure, nerve cells either over-excite other cells, or stop them from sending the right messages to the rest of the body. Epilepsy is diagnosed when these seizures materialize repeatedly.
When you see a Central Maine neurologist about your seizures, you’ll undergo an EEG (electroencephalogram), which can “see” the electrical activity in your brain and, possibly, predict if you’ll keep having seizures. The EEG might find seizure-causing activity in just one part of your brain, or across the entire organ. We might use a process called “cortical mapping” to measure functions and activity in precise spots.
Our Team Approach to Treating Seizures: Because there are so many approaches to seizure control, the Neurology team at Central Maine will form a multidisciplinary team to treat your epilepsy. We’ll take care of your disorder from every possible angle, and professionals guiding your recovery might include nutritionists, neurologists, surgeons and other specialists.
Medications: This is the most widely used treatment. Anti-seizure drugs succeed in controlling seizures for seven out of 10 patients.
Diet: Research has found that a low carb, “keto” diet can control seizures in some people, so your doctor or nutritionist probably will recommend you cut your carbohydrates and focus on eating whole foods, including healthy fats.
Neuromodulation: Your neurologist might also prescribe a device that sends a small electric current to your nervous system. This electric stimulation, called “neuromodulation,” can prompt your brain to release chemicals that change the way your cells act.
Movement Disorders
About a million people in the U.S. live with Parkinson’s disease, and millions more suffer from other movement disorders. They affect every aspect of your life — your job, socializing, mobility, even relaxing with your family. But treatment for movement disorders has come a long way in the last decade, and Central Maine Healthcare is on the leading-edge of movement disorder treatment.
What Are Movement Disorders? If you don’t have a movement disorder, you’ve seen it in others — their heads and limbs jerk or twist in an unnatural way, it may be difficult to understand their speech, and they may not be able to walk.
Parkinson’s disease is a slowly progressing disorder of the nervous system. People with Parkinson’s may not be diagnosed until years after their first symptoms appear. In addition to tremors, people with Parkinson’s also develop problems with their balance, limbs stiffening and slower movements.
Dystonia isn’t as well-known as Parkinson’s, but more than 300,000 people in the U.S. have been diagnosed to date. The muscle contractions with dystonia are different from other movement disorders, in that they cause twisting, repetitive movements. Dystonia can affect the whole body or just one limb.
Other movement disorders include:
- Cervical dystonia, causing twisting contractions of the neck muscles
- Ataxia, when the parts of the brain that control body movements don’t function correctly
- Chorea, marked by brief, irregular movements in the face, mouth, trunk and limbs
- Huntington’s disease, bringing uncontrolled movements, impaired thinking ability and psychiatric disorders
- Restless leg syndrome, when you have an urge to move your legs at night
- Tremors, rhythmic shaking of your hands, head and other body parts
- Wilson’s disease, a rare illness caused by copper build-up in your body, causing neurological problems
Treating Movement Disorders: Your movement disorder may be more easily controlled than you think. Your doctor’s first prescription is likely to be L-Dopa, an amino acid closely related to the brain chemical dopamine and the gold standard for treating Parkinson’s and dystonia, both of which respond to dopamine. Your neurologist at Central Maine also might inject you with Botox®. Botox® temporarily paralyzes muscle activity, making it useful in controlling contractions, especially neck spasms.
Increasingly, surgeons are turning to Deep Brain Stimulation (DBS), a surgery in which electrodes are implanted in the brain. The electrodes produce electrical charges that regulate your brain’s abnormal impulses, controlled by a pacemaker-like device implanted in your chest. A tiny wire connects the “pacemaker” to the electrodes in your brain. DBS is a revolutionary new procedure whose use will go far beyond treating movement disorders; researchers are studying the possibilities of DBS for stroke recovery and dementia, among other conditions.
Central Maine Healthcare can help you minimize and control your tremors and contractions, so you can return to work and regular daily life.
Multiple Sclerosis
Multiple sclerosis (MS) is an autoimmune disease. That means your immune system, which is supposed to protect your from “foreign” invaders (bacteria, viruses, even allergens) instead turns traitor and breaks down your immunity. Those invaders get into your body, and the protective covering that surrounds your nerve cells becomes inflamed, destroying the cells’ ability to work correctly. That’s when you start seeing symptoms of MS.
Central Maine’s neurologists bring on the latest research and techniques to treating your symptoms. When your MS is treated early, you can expect a normal life expectancy, symptom-free — but you must take action.
Diagnosing Multiple Sclerosis: MS is one of the most difficult illnesses to diagnose because its symptoms are almost universal. Anyone can get MS, though women are more likely, and while the typical age at the onset is 20 to 40 years old, it can begin at any age. Diagnosis also is tricky because MS symptoms appear in degrees, from mild (numb limbs, for example) to severe cases with paralysis and blindness. Other symptoms include:
- Blurred or double vision
- Blindness in one eye
- Red/green color distortion
- Muscle weakness in limbs, causing balance and coordination problems
- Prickling, numbing feelings in arms and legs
- Pain in limbs
- Trouble speaking
- Tremors
- Dizziness
- Hearing loss
- Depression
- Difficulty concentrating, and problems with memory and judgement
Some symptoms happen briefly and pass, while others persist. People with MS can be symptom free and then suffer a relapse or flare-up, or the disease can be a steady progression. There’s just no such thing as a “normal” case of MS.
There also is no standard test for MS. Your neurologist and other caregivers will test you based on your current symptoms, and those they think you’re likely to develop. They may give you a neurological exam, blood analysis, brain and spine imaging, lumbar puncture test (known as a “spinal tap”). They also may prescribe an MRI scan, because 90 percent of people with MS show changes in their brain or spinal cord, and other tests that measure magnetic fields of your cells and the electrical activity in your muscles.
Treating You for a Speedy Recovery: There’s no cure for MS, but there is recovery from flare-ups, and that’s our goal when we treat MS at Central Maine. We aim to manage your symptoms, and your treatment will reflect your experience. For instance, we might prescribe a corticosteroid medication such as prednisone to reduce the inflammation in your nerves. We often turn to a host of meds that might slow the worsening of the disease, or help block the immune system’s attack on myelin, that protective covering around your nerves.
If your MS is newly diagnosed or especially severe, we might recommend a plasma exchange. This innovative procedure involves removing your plasma, mixing it with a protein solution, then putting it back into your body. Depending on your symptoms, we might also prescribe meds to combat your fatigue, resolve depression or help control your bowel or bladder. We also prescribe Interferon, a drug that can reduce the severity and frequency of your relapses.
A healthy lifestyle is important, too, in keeping MS symptoms under control. You’ll work with a physical therapist on stretching and strengthening exercises, and you’ll learn to use devices that make daily tasks easier. If you’re feeling stiff or experiencing spasms, we’ll teach you muscle relaxation exercises.
For such a wide range of symptoms, our neurologists will collaborate with as many colleagues as necessary to tame them and get you living a normal, productive life. For most MS patients, there’s no reason not to work full-time and resume all the activities they enjoy.
Stroke
There are 7 million stroke survivors in America today. Central Maine Healthcare treats more than 200 stroke patients each year, mostly through our Emergency Department where we can quickly evaluate and treat your condition. Once you’ve had a stroke or heart disease, your risk of stroking escalates.
If you or a family member are at risk for a stroke, we can help you make sure there are no strokes in your future.
