Angioplasty
Angioplasty, also known as percutaneous coronary intervention, or PCI, is a minimally invasive procedure performed to restore blood flow to the heart muscle when the coronary arteries are partially or entirely blocked. During an angioplasty, a catheter with either a balloon or laser tip is routed to the site of the blockage to clear the artery.
Why Do You Need Angioplasty? The coronary arteries are responsible for carrying blood and oxygen to the heart muscle. When those arteries become blocked, either partially or entirely, by plaque or a blood clot, blood flow is disrupted and your heart doesn’t get the enriched oxygen it needs to pump effectively. In some cases, blocked arteries are discovered as part of routine diagnostic testing, but in other cases, a blockage may be discovered when a patient experiences chest pain and is in an emergency setting.
Getting Ready for Angioplasty: Angioplasty can be performed as an elective (scheduled) procedure when noninvasive testing reveals probable heart disease, or it can be done on an emergency basis to clear blockages during a heart attack. Prior to elective angioplasty, your provider will give you specific instructions about when you’ll need to stop eating or drinking before arriving at the hospital. You may have a blood test that provides information about how fast your blood clots, and you may also get a sedative to help you relax before the procedure.
When angioplasty is performed on an emergency basis, hospitals try to perform the procedure within a 90-minute window after a patient arrives at a hospital with chest pain and other symptoms. Because of this, there really aren’t any steps to take to prepare for emergency angioplasty.
What to Expect During Angioplasty: During angioplasty, the arteries in your heart will be reopened. You will be awake but sedated during the procedure, which is performed in a cardiac catheterization lab. To begin the procedure, your provider will insert a catheter into an artery and then guide the catheter up and into the blocked coronary artery. The provider uses an X-ray and dye to properly visualize the arteries and safely guide the catheter into place.
Once the blockage is reached, your provider will use one of two primary methods to remove the blockage. In one method, a balloon will be inflated at the tip of the catheter, which pushes the plaque causing the blockage to the side, while in the other method, a laser is used to dissolve the plaque. If the blockage in your coronary artery is severe — typically when at least 70% of the artery is blocked — your provider will also likely place a stent in the artery during the angioplasty. A stent, which is made of mesh, holds the artery open and ensures that it does not become blocked again.
Recovering From Angioplasty: Following angioplasty, you will need to remain in the hospital for observation at least overnight. In cases where a stent is placed, you may require a longer hospital stay. Most people are able to return to work and normal activities within a week or so, but your provider will provide individualized guidance about when it’s safe for you to resume normal daily activities. Your post-angioplasty care will also include education and guidance related to heart-healthy habits. Practicing healthy lifestyle habits, including regular exercise and a diet low in saturated fat, will help limit the risk of additional blockages in the future.
Ankle-brachial Index (ABI)
The ankle-brachial index is a simple, noninvasive test to check for peripheral artery disease (PAD). It’s a quick outpatient test that measures the blood pressure at your ankle compared with the blood pressure at your arm. The results are determined by dividing the blood pressure in an artery of the ankle by the blood pressure in an artery of the arm. A low ankle-brachial ratio or index number can be an indication of PAD.
Why Do You Need an Ankle-Brachial Index? Your provider may order an ankle-brachial index if you have leg pain while walking or have any of the following risk factors for PAD:
- Being older than age 70, or being younger than 50 with diabetes and one additional risk factor
- Diabetes
- High blood pressure or cholesterol
- Smoking
The test can also be done to check the severity of PAD if you’ve already been diagnosed. It may be something your provider orders annually.
Getting Ready for an Ankle-Brachial Index: Minimal preparation is needed for this test. You may want to wear loose clothing so the technician can easily place the blood pressure cuffs on your arm and ankle. When you schedule your appointment, ask if there are any additional instructions you may need to follow before your test.
What to Expect During an Ankle-Brachial Index: You’ll need to rest for at least 15 to 30 minutes before the procedure. During the test, you will lie on the table while a technician measures your blood pressure in both arms and both ankles. Testing generally lasts 10–20 minutes, depending on how many times your blood pressure is taken. The technician will calculate the results by dividing the blood pressure in your ankle by the blood pressure in your arm. A low ratio indicates potential PAD. These results will be shared with your provider, who will share them with you. Depending on your provider’s schedule, you may or may not receive the results that day.
Cardiac Catheterization Lab
If you have problems with the muscle, valves or arteries in your heart, Central Maine Heart and Vascular Institute (CMHVI) Cardiac Catheterization Lab is here to provide you with the care you need. At our Cardiac Catheterization Laboratory, also known as the Cath Lab, cardiologists and a team of specialty nurses and radiologic technicians use a procedure known as cardiac catheterization to diagnose, assess and treat heart problems such as coronary artery disease and angina.
State-of-the-Art Catheterization Technology: CMHVI’s Cath Lab uses the latest technology to assess and treat heart problems, including a multi-view camera that rotates around the patient and provides multiple views. This advanced camera emits less radiation than traditional imaging technology, requires less contrast dye and greatly enhances image quality. We also use a cutting-edge hemodynamic system that monitors your blood pressure, the electrical activity in your heart, your pulse and blood oxygen levels during catheterization procedures.
Cardiac Catheterization From Diagnosis to Treatment: Providers use catheterization to perform a variety of procedures, including a type of X-ray called a coronary angiogram that can detect blockages in the arteries. During catheterization, a cardiologist inserts a catheter (thin plastic tube) through an artery in your groin or arm and guides it into your heart. Contrast dye injected through the catheter allows blood vessels to show on a monitor. This part of the procedure is called an angiogram. The test also measures blood pressure and blood oxygen levels. Images from the test detect blockages that may need to be repaired. If an angiogram shows that your arteries are narrowed, you may be a candidate for treatment called percutaneous coronary angioplasty (balloon angioplasty) to reopen them and improve blood flow to your heart. Balloon angioplasty is also used in emergencies to treat patients who have suffered heart attacks because an artery has developed a total or near-total blockage.
Percutaneous Coronary Angioplasty (Balloon Angioplasty): To re-open narrowed or blocked coronary arteries in someone with coronary artery disease or heart attack (myocardial infarction), an interventional cardiologist guides a catheter to the site where a waxy substance made of cholesterol and other substances called plaque has formed a blockage. The tip of a catheter used in this procedure is equipped with a tiny deflated balloon. Once the catheter is in place, the surgeon inflates the balloon. As the balloon expands it pushes aside the plaque, widening the flow space inside the artery. Once the artery is open, the surgeon slowly withdraws the catheter.
Coronary Artery Stent Placement: Once a narrowed or blocked artery has been re-opened, the danger isn’t necessarily over. Arteries that have been unclogged often narrow or close again later. To reduce the risk for this problem, providers often choose to insert a device called a stent in the segment of an artery that was reopened. A stent is a tiny mesh tube that providers implant in an artery to prevent plaque from blocking the blood vessel. Stents are implanted in arteries in the heart (coronary arteries), neck (carotid arteries) or liver. Drug-eluting stents are coated with medication that is released over time to help prevent the artery from becoming blocked again. A coronary artery stent implant may lower the risk of heart attack and stroke.
Other Cath Lab Procedures available at CMHVI Cath Lab:
- Intravascular ultrasound
- Intra-aortic balloon pump
- Pacemaker placement
- Procedural education
- Diagnostic peripheral arterial catheterization
- Percutaneous peripheral arterial intervention (stent placement, angioplasty, limb salvage)
- Diagnostic and intervention peripheral arterial procedures
Cardiac MRI
Cardiovascular Magnetic Resonance Imaging: Cardiovascular magnetic resonance imaging, or Cardiac MRI is a state-of-the-art technique for taking pictures of the heart. It is an imaging modality that can be used to supplement other imaging modalities such as echocardiography and Cardiac CT, but with better accuracy and more detail.
The study is done by asking a patient to lie flat in a strong magnet. One of the more significant patient benefits is that no radiation is used in the study. The magnet emits radio frequency pulses. Based upon the interaction of the impulses, the molecules in the heart and the magnetic field, images are acquired of the heart and displayed on a computer. Using special software, those images are manipulated to provide information about the patient’s heart. Most patients are given a contrast agent through an IV which enhances the image quality and helps increase diagnostic yield. Tissue characteristics of Cardiac MRI are excellent and, as a result, the heart muscle can be closely evaluated for abnormal thickness or cardiac anatomy. Cardiac MRI can also be used to measure the extent of damage, or scar, within the heart muscle that may result from a heart attack. Inflammation of the heart muscle such as myocarditis or pericarditis can be seen in Cardiac MRI as well.
Doppler Ultrasound
A Doppler ultrasound is an imaging test used to evaluate the way blood moves through the blood vessels. It is the only imaging test able to show blood flow and helps providers diagnose vascular disease or determine the success of treatments for arteries and veins. There are different types of Doppler ultrasound, but all use the Doppler effect (an increase or decrease in wavelength) to measure sound waves that reflect off of moving blood cells to create an image.
Why Do You Need a Doppler Ultrasound? Doppler ultrasounds help your provider find out if your blood flow is blocked or reduced. These imaging tests can help diagnose conditions such as:
- Arteriosclerosis
- Carotid arterial stenosis
- Deep vein thrombosis
- Peripheral artery disease
- Venous insufficiency
Getting Ready for a Doppler Ultrasound: Depending on the type of Doppler ultrasound your provider orders, you may not be able to eat or drink for several hours before. If you smoke, avoid cigarettes or other nicotine products at least two hours before your test. Nicotine causes your blood vessels to narrow, which may affect your test results.
What to Expect During a Doppler Ultrasound: First, a radiologist or ultrasound technologist will put a gel on the skin of the area being tested. This gel helps sound waves travel between a transducer, which sends sound waves into your body, and your skin. As the transducer travels over your skin, moving blood cells will cause the pitch of the sound waves to change. The sound waves are recorded on a computer and made into graphs or pictures, depending on the type of Doppler ultrasound performed. The test usually takes 30 minutes to an hour to complete. After your test, the radiologist or technologist will send your results to a provider. The provider will review your results and, if necessary, alert you of any next steps.
Echocardiogram
An echocardiogram is a type of ultrasound imaging that uses high-frequency sound waves to make a detailed picture of your heart on a video monitor. Echocardiograms look at your heart’s blood vessels, chambers, valves and walls. They allow your provider to see the size and shape of your heart, how your heart moves and pumps blood, and whether your heart valves are working correctly.
Why Do You Need an Echocardiogram? Your provider may recommend an echocardiogram to check your heart’s function or to see how your heart looks. An echocardiogram can be used to detect many heart problems, such as:
- Abnormal heart valves
- Damage after a heart attack
- Heart failure
- Heart murmurs
- Infection or tumors in the heart
- Pulmonary hypertension
- Stenosis
Getting Ready for an Echocardiogram: No at-home preparation is necessary for an echocardiogram, and you can eat or drink as you normally do on the days before.
On the day of your echocardiogram, you may find it helpful to wear a shirt or blouse you can easily remove.
What to Expect During an Echocardiogram: During your test, the technician will put a gel on your chest to help the sound waves reach your heart through your skin. A device called a transducer will be placed and moved around on your chest. The transducer transmits ultrasound waves into your chest. The waves will bounce off your heart and “echo” back to the transducer, which will help create the pictures of your heart. The test usually takes less than an hour to complete.
After your echocardiogram, the technician will send the pictures to a cardiologist. The cardiologist will review the pictures and tell you about any next steps you may need to take.
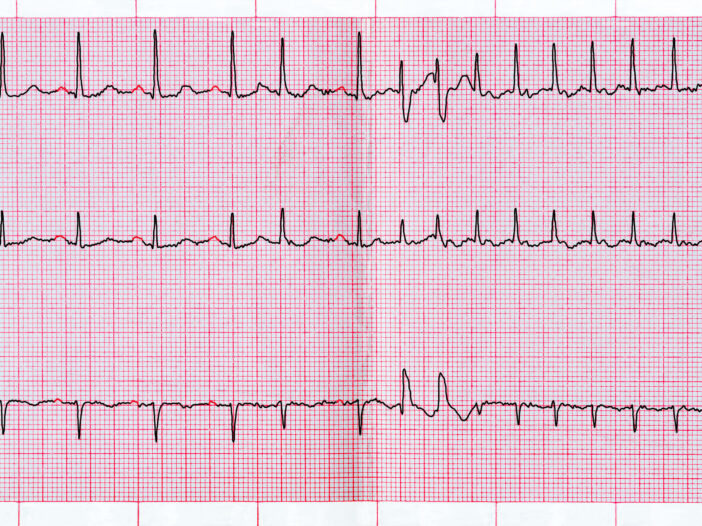
Holter Monitors
A Holter monitor is a device that continuously records your heart’s activity for a short period of time, usually 24 to 48 hours. It works as a portable electrocardiogram (EKG) that measures your heart’s electrical activity. Unlike a traditional EKG that takes only a few seconds worth of data, a Holter monitor gives your provider more detailed information about your heart during normal activity. As you wear the monitor, it measures the speed and regularity of your heartbeat and the strength and timing of your heart’s electrical impulses.
Why Do You Need a Holter Monitor? Holter monitors help providers diagnose arrhythmia (irregular heartbeat) and determine the success of treatments. You may be asked to wear a Holter monitor if you:
- Become faint or dizzy regularly
- Experience irregular heartbeat
- Need to determine whether your heart is getting enough oxygen
- Recently had a heart attack
- Take medications intended to treat a cardiac condition
Getting Ready for a Holter Monitor: Holter monitors generally have small electrodes that attach directly to your chest with adhesive. Wires connect these electrodes to a monitor that you keep in a pocket, hang over your shoulder or wear around your waist. Very little preparation is needed before you wear one. However, you cannot get the electrodes or monitor wet, so you should bathe or shower prior to receiving the device. Men who have hair on their chests may need to shave the area where the electrodes will be placed.
Electricity and magnets can affect the Holter monitor’s readings, so you will need to take some precautionary steps:
- Avoid electric blankets, electric razors, electric toothbrushes, magnets, metal detectors and microwave ovens while wearing the device.
- Do not have any X-rays while wearing your monitor.
- Keep cellphones and other electronic devices, such as MP3 players and tablets, away from the monitor.
What to Expect During a Holter Monitor Test: Wearing a Holter monitor is painless, and you will be free to go about your usual activities. However, you will need to track any symptoms, such as dizziness or unusual heartbeat, in a diary. Note the time and what you were doing when the symptoms occurred. When your test period is complete, you will return your Holter monitor to your healthcare provider. They will then process your test results, which should be ready for you within one to two weeks.
Stress Test
Otherwise known as an exercise test or treadmill test, a stress test demonstrates how well your heart performs under pressure. During physical activity, your body needs more oxygen than it does when it is at rest. In response, your heart needs to pump more blood. The stress test illustrates if an adequate amount of blood has been pumped to the arteries that supply your heart. This test will also help you and your provider understand what kind of exercise is safe for your body.
Why Do You Need a Stress Test? If you have symptoms of a heart complication, including chest pain, dizziness, irregular heartbeat or shortness of breath, your provider may recommend a stress test. This test may help determine if you have a heart condition, such as:
- Heart failure
- Heart valve disease
- Ischemic heart disease
Getting Ready for a Stress Test: Prior to your test,
- Ask your provider if there are any medications you should stop taking.
- Do not drink beverages that contain caffeine, such as soda, coffee or tea, on the day of your test.
- Wear comfortable clothing.
What to Expect During a Stress Test: When you arrive for your stress test, a healthcare provider will inject a radioactive substance into one of your veins. This substance will help your provider see how well blood is flowing into your heart. For about 15 to 45 minutes, you will recline and relax while the substance travels to your heart. The provider will then put electrodes on your chest, a blood pressure cuff on your arm and a pulse monitor on your finger to monitor your blood pressure and heart activity while your body is at rest and as you start to move.
During the actual test, you will walk on a treadmill or pedal an exercise bike with increasing speed and intensity. You may also breathe into a tube for a few minutes as you exercise. Once the test is complete, you will rest while your results are evaluated. Your provider will evaluate several results, including your blood pressure, breathing, heart rate and your level of fatigue.
Vascular Lab Diagnoses Circulatory System Issues
The Central Maine Heart and Vascular Institute’s Vascular Lab uses non-invasive vascular measures to diagnose conditions and abnormalities of the circulatory system, including blood vessel blockages and aneurysms. The Vascular Lab is accredited by the Intersocietal Commission for the Accreditation of Vascular Laboratories. The lab’s sonographers are nationally certified.
24-hour Blood Pressure Monitoring
Recording someone’s blood pressure over a 24-hour period may be done to help diagnose patients experiencing borderline high blood pressure, uncontrollable blood pressure, blood pressure problems caused by medications, pregnancy accompanied by high blood pressure, or fainting spells.
A 24-hour blood pressure monitor is a small digital device that records blood pressure readings while an individual is at home, work or participating in day-to-day activities. This information shows how environmental factors impact an individual’s cardiovascular system, including “white-coat hypertension” experienced by those who only have high blood pressure at the provider’s office. Patients are asked to keep a diary of their activities, so the provider will know when patients were active and when they were resting.
Abdominal Ultrasound
An abdominal ultrasound is a painless test that provides information about internal organs and blood vessels within the abdomen. Sound waves are used to produce images. The ultrasound may be prescribed for patients with kidney, liver, gallbladder, appendix, pancreatic, spleen or arterial issues. The exam may take up to an hour. Patients recline while the technician uses a wand and gel to transmit soundwaves, which are then recorded as images.
Ankle Brachial Indexes (ABIs)
Ankle-brachial index (ABI) testing measures blood pressure in the arms and legs for comparative analysis. The ratio of the two measurements can indicate if there is a blood flow problem in the legs. ABI testing is a non-invasive flow study (NIFS) used to diagnose claudication, experienced as pain while walking, may be caused by peripheral arterial disease (PAD). PAD, a form of atherosclerosis, causes arteries to narrow and leg muscles to receive less blood, and therefore less oxygen.
Diagnosing this condition is important, as it may precede cardiovascular issues, including heart attack or stroke. The test takes 45 minutes to an hour. No special preparation is needed.
Arterial Duplex Ultrasound
An arterial duplex ultrasound is used to evaluate issues involving arteries and/or veins of the arms and/or legs. This painless, non-invasive procedure uses sound waves to gather information. Blood flow is measured and images of the blood vessels are taken. The technician transmits sound waves with the use of a wand that is gently passed over the areas being studied. The procedure takes about an hour.
Carotid Duplex Ultrasound
Carotid duplex ultrasound is a simple and painless procedure that allows providers to evaluate the carotid arteries in the neck. These major arteries supply blood to the brain. When blood flow to the brain is insufficient, a stroke and/or death are possible. The ultrasound may reveal blood clots (thrombosis), narrowing of the arteries (stenosis), or other blockages. The ultrasound uses sound waves to produce images of the blood vessels so blood flow can be evaluated.
Segmental Pressures
Segmental pressure testing is similar to ankle-brachial index (ABI) testing but involves two or three additional blood pressure cuffs. These are placed just below the knee, just above the knee, and at the upper thigh. Blood pressure at each point is recorded. Significant drops between body segments may suggest blockages or narrowing in the arteries.
Segmental pressure testing is a non-invasive flow study (NIFS) used to diagnose claudication, experienced as pain while walking, may be caused by peripheral arterial disease (PAD). PAD, a form of atherosclerosis, causes arteries to narrow and leg muscles to receive less blood, and therefore less oxygen. Diagnosing this condition is important, as it may precede cardiovascular issues, including heart attack or stroke. The test takes 45 minutes to an hour. No special preparation is needed.
Venous Ultrasound Imaging
Venous Ultrasound Imaging captures real-time images of the inside of the body. Venous ultrasound, in particular, looks at blood flow through veins in the arms or legs. Ultrasound is easy-to-use, less expensive than other imaging methods, and does not emit any ionizing radiation. For standard diagnostic ultrasound there are no known harmful effects on humans.
Venous ultrasound studies are used to evaluate varicose veins; assist in the placement of a needle or catheter into a vein; evaluate veins in the leg or arm for potential use for bypassing a narrowed or blocked blood vessel (graft); and examine a blood vessel graft. Venous ultrasound is used to search for blood clots, especially in leg veins. Often called deep vein thrombosis, or DVT, these clots can cause a dangerous condition called pulmonary embolism if they move to the lungs. However, if a blood clot in the leg is detected early enough, proper treatment can prevent it from passing to the lung.
A provider specifically trained to supervise and interpret imaging examinations (radiologist) analyzes the ultrasound results and sends a report to the patient’s primary care provider and/or to the provider who referred the patient for the exam.
